Suture fixation for Olecranon fractures: A Systematic Review
- Corresponding Author:
- Gedion.Y. Amdetsion
Department of Orthopaedics and Trauma, Barts Health NHS Trust, UK
E-mail: gedion.amdetsion@nhs.net
Abstract
Background: Approximately 10% of upper limb fractures involve olecranon fractures. Traditionally, these fractures have been treated with tension band wiring or plate fixation, which often result in a high reoperation rate. To mitigate complications and reduce the need for reoperations, various techniques utilizing sutures or suture anchors have been introduced. The aim of this review is to evaluate the current best evidence on the management of olecranon fractures.
Methodology: In June 2023, relevant randomized controlled trials were systematically collected from databases including PUBMED, MEDLINE, EMBASE, and Cochrane Library. The methodological quality of the articles was assessed using risk of bias assessment tools. The study protocol was registered in the Prospero database with registration number CRD42023436800.
Results: Out of 274 initially identified records, a total of 9 studies were deemed relevant for inclusion. Among them, 7 were case series, 1 was a retrospective cohort study, and the remaining study was a case-control study. These 9 studies involved a total of 257 patients with olecranon fractures, with 49 of the fractures being chevron osteotomies. Among the patients, 101 out of 257 were male, with a mean age of 61.2 years. The follow-up periods in the included studies ranged from 6 months to 7.5 years. Outcome measures varied and included patient-rated and physician-rated measures, as well as radiological outcomes. The analysis revealed that suture fixation demonstrated a low reoperation rate and yielded satisfactory to excellent clinical and functional outcomes.
Conclusion: In summary, based on the currently available evidence, it is not possible to draw definitive conclusions regarding the clinical superiority of suture fixation for olecranon fractures. However, suture fixation does emerge as a viable alternative for treating simple displaced fractures in adults, especially when tension band wire fixation is the conventional approach. Additionally, anchor fixation utilizing Fiber Wire shows significant potential in the treatment of olecranon fractures in elderly patients. Moreover, the findings from this systematic review indicate that suture fixation may help reduce the need for reoperations.
betsat bettilt vegabet betkanyon matbet celtabet hilbet melbet kingbetting wipbet pusulabet superbahis lidyabet holiganbet 1xbet asyabahis jetbahis betdoksan betetebet betgram
Keywords
Olecranon fracture, Elbow fracture, Tension band wiring, Plate fixation, Conservative treatment, Suture fixation, Suture Anchors, Systematic review
Introduction
Olecranon fractures typically result from a direct blow to the olecranon. More complex fracture dislocation patterns may be the result of a more indirect injury such as a fall onto the outstretched hand [1]. Around 10% of fractures in the upper extremity are olecranon fractures [2]. The incidence rate is approximately 12 cases per 10,000 individuals. On average, these fractures occur at the age of 57, with males being more prone to experiencing them at a younger age. Olecranon fractures often coincide with other elbow injuries, particularly involving the radial head and coronoid. Open fractures account for approximately 6.4% of these injuries [3].
The Mayo classification divides olecranon fractures into three groups based on fracture displacement and elbow stability. These groups include type I (undisplaced), type II (displaced but stable), and type III (unstable). Each group is then subdivided into comminuted (A) or noncomminuted (B) fractures. This classification helps direct treatment with type I generally being amenable to nonoperative management while type II and III fractures generally require operative treatment. Type B fractures are more suitably treated with plate fixation while type a fractures may be treated with tension band constructs if preferred [4].
Tension Band Wiring (TBW) is the commonly employed method for tension band constructs,specifically suitable for transverse fractures with minimal damage to the joint surface and no signs of instability between the ulna and humerus. Although this technique generally leads to successful fracture healing, it is important to note that there is a relatively high rate of reoperations associated with it. The most prevalent complication observed in this procedure was the symptomatic protrusion of the Kirschner wires at the elbow. Additionally, other complications included skin breakdown and infection [5].
Alternative approaches such as plate fixation have lower risk of wire migration, but they come with their own unique complications and require more expensive implants compared to Tension Band Wiring (TBW) [6]. Specifically, dorsal plates can lead to discomfort and difficulties in wound healing, particularly in patients with slender body build or delicate soft tissues, when pressure is applied to the elbow [7].
Various techniques involving sutures or suture anchors have been introduced to minimize complications related to hardware and the need for reoperations. One such technique, initially described by Ravenscroft et al., involves using synthetic sutures exclusively to secure the fracture. Watts et al. further developed this concept by introducing an all-suture technique. Tension suture repair is believed to decrease the likelihood of requiring a subsequent surgery to remove the fixation material. Introducing an intervention that is at least as effective as the current method in terms of patient function, while also reducing the necessity for a second surgical procedure, would significantly benefit patients. This approach would not only alleviate patient discomfort and the need for reoperation but could be cost-saving [8].
This study was aimed to examine the clinical effectiveness of tension suture or anchor repair in comparison to traditional tension band wiring for surgically fixing Mayo grade I and II olecranon fractures. The main objective was to assess and compare the functional and clinical outcomes as the primary measure. While also analyzing the rate of complications, reoperation, and radiographic union to make a comparison.
Methodology
We conducted an online systematic literature search in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. It was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO: CRD42023436800).
We systematically searched for studies of olecranon fracture that reported the clinical and/or radiological outcome of tension/anchor suture repair compared with other modalities. PUBMED, MEDLINE, EMBASE, and Cochrane Library databases, were searched from inception to the date the search was performed (25/6/2023). The computer based searches terms such as Olecranon and on the other side terms such as (tape, anchor, tension band suture, and suture) were used. No language restrictions were used. Reference lists of retrieved articles and review articles were manually scanned for all relevant additional studies.
■ Criteria for including studies
• P: adults above 18 with Mayo I and II olecranon fracture requiring surgical fixation.
• I: Tension suture repair.
• C: Wiring and plating.
• O: reoperation rate, elbow function.
■ Study design
Case series more than 2, retrospective and prospective cohorts, RCT
Results
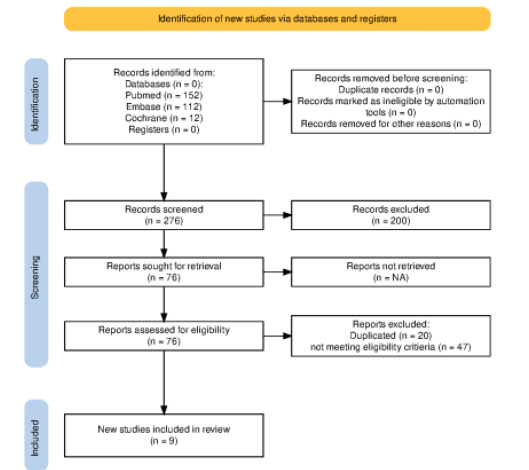
Following the utilization of the aforementioned search items, a comprehensive tally of 274 studies was identified. Subsequently, through the meticulous application of our inclusion and exclusion criteria, a total of 9 relevant studies were deemed suitable for our review. Owing to the fact that our primary focus lay on functional and clinical outcomes, which cadaveric models inherently fail to elucidate, the decision was made to omit cadaveric studies from our analysis (Figure 1).
Upon thorough examination of the reference lists and author contacts associated with these pertinent articles, no additional studies were uncovered. Independent analysis of the complete texts of all the identified articles ultimately yielded no further studies that could be incorporated into the final review. Amongst the selected studies, 7 constituted retrospective case series, while 1 was a case-control study, and the remaining one was a retrospective cohort study
All of the identified articles were categorized as level III or IV in accordance with the NHMRC levels of evidence. Regrettably, at the time of the review, no randomized controlled trials of level 1 were available. However, it is worth noting that ongoing randomized controlled trials were identified during the course of our investigation. The cumulative size of our cohort under scrutiny encompassed 257 individuals, with an average age of 60.9 years. Furthermore, it is important to acknowledge that one of the included studies disclosed potential conflicts of interest in relation to their research (Table 1).
Table 1: Risk of bias assessment.
| Study | Research type | ROB assessment |
|---|---|---|
| Gu et al (25) | Case series | Moderate: Small sample case series; no comparison between suture types |
| Phadnis et al (19) | Cohort | Moderate: No functional scores, Uneven distribution of cases between groups, had osteotomies |
| Crozier-shaw et al(23) | Case control | Moderate: Small sample size, No functional scores, potential for confounders |
| Garcia-Elvira Et al(24) | Case Series | Moderate: Small sample case series; no control; |
| Das et al(22) | Case Series | Moderate: Small sample case series, No control |
| Bateman Et al(20) | Case Series | Moderate: Small sample case series; no comparison between suture types; |
| Wagener et al(21) | Case Series | Moderate: Small sample case series; no comparison between suture types; no functional scores; Chevron osteotomies performed. |
| Cha et al(26) | Case Series | Moderate: Small sample case series; No comparison, open fractures in most cases; funding of study. |
| Xu et al(27) | Case Series | Moderate: Small sample case series; no comparison between suture types; no functional scores; |
We then proceeded to do Risk of bias assessment using Murad et al (2018) for case series and ROBINS-I tool for nonrandomized studies (controlled/cohort/case-control etc.).
Considering most of the studies included were case series, we felt we wouldn’t be able to perform a statistically meaningful quantitative analysis, nevertheless, we provide the result of the selected studies as follows:
■ Demographics
The 9 included studies contributed a total of 257 patients with olecranon fractures; 49 of these fractures were chevron osteotomies; 101/257 of patients were male, with mean ages of 61.2 years Amdetsion, et al
■ Follow up
In all, 9 studies reported their follow up period, ranging from 6 months to 7.5 years.
■ Fracture classification
All of the 9 included studies followed the Mayo classification of olecranon. 199 of the included patients had Mayo 2A fracture type, while 5 were Mayo 3A, and 18 were Mayo 2B. Bateman et al. didn’t provide clear data on the proportion of patients who had Mayo 2B fracture types. Meanwhile, 49 of the included cases were patients who had chevron osteotomy
■ Assessment of clinical outcomes
Four studies used recognized clinical outcome scores (Quick DASH, 12 DASH, 13 Mayo Elbow Performance Score (MEPS) 10, and Oxford elbow score). Interestingly, all of them were reported in the good to excellent ranges. While four studies, opted to describe functional outcomes in terms of Range of motion with all four reporting all their patients had Range of motions: flexion greater than 100 degrees and full extension with only one patient in the CrozierShaw et al. Cohort study having an extension lag of 15 degrees. However, the Phadanis et al study didn’t report any type of functional outcome [9].
■ Assessment of radiological outcomes
ll of the studies used a combination of nonunion/malunion, delayed union, fracture consolidation, to report radiological outcomes. One study, Xu et al did not state how or whether radiological outcomes were assessed. Phadanis et al reported one non unions, it explained it might be because the patient had osteotomy “Anecdotal experience suggests that osteotomies take longer to unite than an acute fracture”. While GarciaElvira et al, reported 7 patients with good anterior union but posterior diastasis [10-24].
■ Complications
All 9 studies reported on the complication rates. With Garcia El Avira et al, reporting 3 wound infection of which two required surgical debridement and one pseudo arthrosis managed conservatively. .Xu et al, reported one removal of suture due to prominence of the suture knot and Phadanis reported one failed fixation, which is suspected to be due to technical error. As there “was propagation of the transverse ulnar tunnel through the dorsal cortex resulting in loss of suture tension. This was attributed to a technical error in placing the transverse tunnel too close to the dorsal cortex” [24]. However, the overall reoperation rate for suture fixation was 5% with only 2.4% of patients requiring refixation. While, the overall reoperation rate in the included studies for the TBW group was 38%, with the main reason being prominent wire (Table 2) [19].
Table 2: Review of articles
| Study+A1 :L15 | Research type | Number of patients | Surgical Procedure for Cohorts | Sex | Age(S+_) | associated condition | Fracture classificatio | material used detail | Radiological Union | Functional Outcome | Complication |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gu et al (25) | Case series | 12 |
3 |
51.1 |
3 Mayo 2a, 9 2B | two 3.5 mm anchors (Smith & Nephew, US) | 3: 4-6 weeks | Mayo Elbow score: 4: 92-95 | no complications | ||
| Phadnis et al(19) | Case series | 168 |
overall | 71/95 |
55 |
131 Mayo IIA, 7 Mayo 1, 30 Chevron Osteotomy | 6-16 weeks | Overall complication: reoperation22%(37), 30 for prominent hardware, 4 for infection, 3 for failed fixation | |||
| TBW: | osteotomy: 8,Mayo I:5, Mayo II:76 | 2 2 mm longitudinal K , 18 gauge figure of eight steel wire |
reoperation:36%(26: prominent hardware, 4 for infetion, 2 failed(circumstance Mayo 2b and distal humeral ostetomy)) |
||||||||
| Suture | osteotomy:17, MI: 2, Mayo 2: 22 |
2 number 2 Orthocord suture | reoperation:2%(1: failed): circumstane distal humeral fracture ostetomy technical error , 1 non untion, also possible technical error |
||||||||
| Plate | osteotomy:5, Mayo 1 :0, Mayo 2: 33 |
dorsal pre-contoured peri-articular locking plate and a combination of 2.7 mm and 3.5 mm locking and cortical screws. |
reoperation:11%(4 prominent hardware | ||||||||
| Crozier-shaw et al(23) | Case series | 11 |
Overall | 05-Jun |
56.1 |
||||||
| Suture | 52.4 |
Mayo 2A: 1, Mayo 2B: 2 and Mayo 3A: 1 | Magnezix® compression screw and application of a Neoligaments™ polyethylene band in a figure of 8 to act as a tension band | 4/5 achieved union, 1 lost to follow up |
all patients flex greater than 110 and were able to extend fully except for one patient who had a 15 degree extension lag | ||||||
| TBW | 59.17 |
Mayo 2A: 5 and Mayo 2B: 1 | No limitation in ROM after removal of metal work |
5 were listed for removal of metal work | |||||||
| Garcia- Elvira Et al(24) | Case series | 29 |
Mar-26 |
79 |
No. 5 Ethibond, No. 2 Ultrabraid, No. 2. Orthocord | 24 radiological union at full follow up, 7 non unions, 2 lost to followup but good fucntion |
flexion mean 130, extension: 0 | 3 wound infections, 1 pseudoarthrosis but good range of motion, but two patients required debridement for soft tissue infection, | |||
| Das et al(22) | Case series | 10 |
03-Jul |
47 |
All Mayo 2 A | No 2. Orthocord × 2 | on average all u | DASH 9, oxford 41 | no complication or reportation, | ||
| Bateman Et al(20) | Case series | 8 |
0/8 | 73.5 |
Mayo 2A and 2B | Two 5.5-mm biocomposite fully threaded suture anchors and 2 distal 3.0-mm biocomposite PushLock transosseous anchors |
All united | Quick Dash: 4, OES:47.2 | No complication, no reoperation | ||
| Wagener et al(21) | Case series | 19 |
07-Dec |
62 |
Chevron Osteotom | large cancellous screw with Fibrewire tension suture band | All united by 8 weeks |
No complication, no reoperation | |||
| Cha et al(26) | Case series | 13 |
69.5 |
9 open fracture s Had cardiova cular comorbi dity |
9 Mayo 2A, 4:3 A | Four strands of No. 2 FiberWire with 4.5-mm Bio-PushLock (Arthrex) | Most had union by 3 month, 2 patients had delayed union with union seen at 12 months | Mayo Elbow score 86, DASH 16 | No complication, no reoperation, all united |
Discussion
The systematic review was conducted to assess the functional and radiological outcomes of olecranon fractures treated with suture fixation, as well as the impact of different techniques and the appropriateness of nonmetallic fixation for various fracture types. Data from nine studies involving 257 fractures were analyzed, revealing substantial variability in fracture types, materials used, and outcome assessments. The systematic review identified four key findings based on the Analyzed Randomized Controlled Trials (RCTs). Firstly, there was a notable lack of highquality evidence in the literature regarding the topic under investigation. Secondly, nonmetallic fixations consistently resulted in good functional outcomes across Mayo 2A/B and 3A fractures. Thirdly, chevron osteotomy didn’t show a higher complication rates. Lastly, Anchor suture fixation had better outcome in fixation of olecranon fracture in the elderly and likely osteoporotic bone. Unfortunately, the available evidence did not allow for pooling the results to conduct a more accurate meta-analysis. All studies that utilized clinical outcome scores or Range of motions assessment reported positive functional, clinical, and radiological outcomes in patients treated with nonmetallic fixation. These patients achieved satisfactory to excellent functional scores and/or adequate range of motion, with most fractures successfully united and only a few cases experiencing delayed union or non-union. One study by Phadanis et al which employed two No. 2 orthocord wires, suggested that patients who underwent chevron osteotomy were more likely to experience delayed union [19]. However, another study by Wagener. Utilizing large cancellous screws with fiber Wire, reported good radiological and clinical outcomes in all patients who underwent osteotomy. It is worth mentioning that Fiber Wire exhibited an ultimate strength up to 2.5 times greater than traditional non-absorbable sutures like polyester or polydioxanone, as demonstrated by several biomechanical studies that found its strength comparable to stainless steel [15, 16]. The use of high-strength braided sutures, such as No. 5 Ethibond, No. 2 Ultrabraid, and No. 2 Orthocord also proved effective in maintaining fixation and reducing reoperation rates. However, these sutures showed some failure at high forces during simulated early mobilization. When considering fracture union, it is important to give special attention to osteoporotic bones, as indicated by two studies involving participants with a mean age above 70. In Garcia Elvira et al, 7 out of 29 patients experienced delayed or nonunion. All patients in this study were treated with ethibond /Ultrabraid/orthocord. In contrast, Bateman et al. reported no complications, with all 8 patients achieving radiological union [20, 24]. These patients were treated with anchor sutures. These findings align with a study conducted on an osteoporotic cadaveric model, which suggested that suture anchor fixation may be suitable for early rehabilitation compared to the traditional tension band technique with K-wire fixation. It should be noted that polyester suture fixation proved inferior as it failed after an average of 17 cycles during the push-up technique and exhibited significantly higher displacement compared to the other two methods [18]. This could potentially explain the occurrence of non-union, as the fixation might not have provided sufficient stability. However, it is important to acknowledge that we currently lack sufficient data to draw any conclusive statements. Interestingly, even patients who developed complications such as infection or non-union exhibited good range of motion. Additionally, several studies on patients treated with tension band wiring or plating consistently demonstrated relatively positive clinical outcomes. The drawback of metallic fixation was the higher complication rate, necessitating removal of the fixation even after fracture union. In spite of the complications, after removal of the wire the patients had good functional outcomes. Illustrating, the non-inferiority of suture fixation when compared to TBW. Complications following operative treatment with tension band wiring were common, primarily due to hardware prominence under the thin soft tissue coverage of the olecranon. It is unsurprising that hardware prominence remained the most common adverse effect, with a review reporting a re-operation rate of 27% [14]. However, the cases reviewed in this study consistently showed a lower rate of reoperation in suture fixation, with an overall reoperation rate of just under 5%. Notably, the overall reoperation rate in patients who underwent olecranon chevron osteotomy following suture fixation was also 5%, indicating relatively positive outcomes despite a moderate risk bias observed in both articles. Cha S. et al, included patients with open fracture and medical comorbidities which generally tend to increase the risk of infection yet there was no reoperation or wound infection. Interestingly, Garcia-Elvira et al reported 3 wound infections with 2 of them requiring superficial debridement. The fact the infection wasn’t deep shows there was no biofilm on the fixation and the infection is probably unrelated to the fixation used [24- 27]. This systematic review tried to provide an in-depth examination of the functional and clinical outcomes of suture fixation in olecranon fractures. All the included studies consistently reported positive results in terms of fracture reduction, patient functional outcomes, and reduced complications, thereby minimizing the need for subsequent surgical interventions.
Conclusions
In conclusion, the available evidence is insufficient to establish robust conclusions regarding the clinical superiority of one treatment modality over another for olecranon fractures. However, suture fixation appears to be a valid alternative for treating simple displaced fractures in adults, especially in cases where tension band wire fixation would typically be used. Moreover, the cumulative results of this systematic review suggest that suture fixation may reduce the rate of reoperation to remove traditional metalwork, thereby potentially lowering healthcare costs. Moreover, Anchor fixation with Fiber Wire had a higher radiological union rate and less complication in fixation of osteoporotic bones. Further high-quality randomized controlled trials involving human participants are necessary. During the review, ongoing randomized control studies were identified, and it is anticipated that repeating the systematic review upon their completion will allow for a quantitative analysis and the generation of robust recommendations.
References
- Rockwood Jr, D. P , R. W. Rockwood and Green’s fractures in adults. Ed. CA. 511-3 (1997).
- Wiegand, Laura, Joseph Bernstein, et al. Fractures in brief: olecranon fractures. Clin. Orthop. Relat. Res. 470, 3637-3641 (2012).
- Duckworth AD, Clement ND, Aitken SA, et al. The epidemiology of fractures of the proximal ulna. Injury. 43, 343-346 (2012).
- MORREY, Bernard F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. JBJS 77, 316-327 (1995).
- Macko, D. O. N. A. L. D, and R. M. Szabo, et al. Complications of tension-band wiring of olecranon fractures. JBJS. 67, 1396-1401 (1985).
- Amini MH, Azar FM, Wilson BR, et al.. Comparison of outcomes and costs of tension-band and locking-plate osteosynthesis in transverse olecranon fractures: a matched-cohort study. Am J Orthop. 44, E211-5 (2015).
- Claessen FMAP, Braun Y, Peters RM, et al.. Factors associated with reoperation after fixation of displaced olecranon fractures. Clin. Orthop. Relat. Res. 474, 193-200 (2016).
- Das, Abhishek K., Arpit Jariwala, et al. Suture repair of simple transverse olecranon fractures and chevron olecranon osteotomy. Tech. Hand Up. Extrem. Surg. 20, 1-5(2016):.
- Murad MH, Sultan S, Haffar S, et al. Methodological quality and synthesis of case series and case reports. BMJ evid.-based med. (2018).
- Cusick MC, Bonnaig NS, Azar FM, et al. Accuracy and reliability of the Mayo elbow performance score. J. hand surg. 39, 1146-1150 (2014):.
- Dawson, J., Doll, H., Boller, et al. Specificity and responsiveness of patient-reported and clinician-rated outcome measures in the context of elbow surgery, comparing patients with and without rheumatoid arthritis. Orthop. Traumatol.: Surg. Res. 98.6 (2012):.
- Beaton, Dorcas E. BScOT, et al. Development of the QuickDASH: comparison of three item-reduction approaches. JBJS 87.5 (2005): 1038-1046.
- Gummesson, Christina, Isam Atroshi, et al. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC musculoskelet. disord. 4, 1-6 (2003).
- Rantalaiho IK, Miikkulainen AE, Laaksonen IE, et al. Treatment of displaced olecranon fractures: a systematic review. Scand. J. Surg. 110, 13-21 (2021).
- Wu¨st DM, Meyer DC, Favre P,,t al. Mechanical and handling properties of braided polyblend polyethylene sutures in comparison to braided polyester and monofilament polydioxanone sutures. Arthrosc.: J. Arthrosc. Relat. Surg. 22, 1146-1153(2006).
- Carofino, Bradley C, Browner BD, et al. Olecranon fractures repaired with FiberWire or metal wire tension banding: a biomechanical comparison. Arthroscopy: Arthrosc.: J. Arthrosc. Relat. Surg. 23, 964-970(2007).
- Von Keudell A, Kachooei A, Mohamadi A, et al. Efficacy of early surgery and causes of surgical delay in patients with hip fracture. j. orthop. 12, 142-146 (2015).
- von Keudell A, Kachooei A, Mohamadi A, et al . Biomechanical properties of an intramedullary suture anchor fixation compared to tension band wiring in osteoporotic olecranon fractures- A cadaveric study. J Orthop.17, 144-149(2019).
- Phadnis, Joideep Sunil, Watson, et al. Comparison of all suture fixation with tension band wiring and plate fixation of the olecranon. J. Shoulder Elb. Surg. 12. 414-421. (2020).
- Bateman, Dexter K., VanBeek, et al. Suture anchor fixation of displaced olecranon fractures in the elderly: a case series and surgical technique. J. Shoulder Elb. Surg. 24. 1090-1097 (2015).
- Das, A. K., Jariwala, A., Watts, A. C, et al. Clinical results of the re-fixation of a Chevron olecranon osteotomy using an intramedullary cancellous screw and suture tension band. Strateg. Trauma Limb Reconstr. 10, 1-4 (2015).
- Das, Abhishek K., Arpit Jariwala, et al. Suture repair of simple transverse olecranon fractures and chevron olecranon osteotomy. Tech. Hand Up. Extrem. Surg. 20,1-5 (2016).
- Crozier-Shaw, Geoff, John Mahon, et al. The use of bioabsorbable compression screws & polyethylene tension band for fixation of displaced olecranon fractures J. Orthop. 22, 525-529 (2020).
- García-Elvira, Ruben, Camacho-Carrasco, et al. Olecranon mayo IIA fractures treated with transosseous high strength suture: a series of 29 cases. Injury 51,S94-S102 (2020).
- Gu, Pei-feng, Chen, et al. Surgical technique and analysis of functional results of anchor for the treatment of olecranon fracture. Asian j. surg. 46, 1336-1338 (2023).
- Cha, Soo Min, Hyun Dae Shin, et al. Application of the suture bridge method to olecranon fractures with a poor soft-tissue envelope around the elbow: Modification of the Cha-Bateman methods for elderly populations. J. Shoulder Elb. Surg. 25, 1243-1250 (2016).
- Xu, Sheng, Heng An Lin, et al. Repair of comminuted (Mayo type IIB) olecranon fracture using Ethi-bond 5 sutures without metallic implants: A novel technique. J. Orthop. 16, 329-333 (2019).