Sniffing 'infection odour': A cross sectional study of odours from patients with infectious disease
- Corresponding Author:
- Dr. A Sridhar
Resident in Neurology
Department of Neurology
Government General Hospital
Guntur-522002, India
Tel: +91-8985183641
E-mail: iamimenotu@gmail.com
Abstract
Background
Infectious diseases are associated with many types of odours emanating from the host. But data on ‘infection odour’, i.e. the smell common to most infections has not been studied. We investigated to find any such physician identifiable odour [infection odour] common to the process of infection which might provide a valuable clue to the diagnosis of infectious disease.
Methods
Over a one month period in the Tertiary Govt. General Hospital, Guntur, India, the study physician approached 52 hospitalised infected patients and 61 non infected patients to detect the smells emanating from them. During the process of clinical examination the smell emanating was noted by the physician. Data on clinical profile, nature and severity of illness were also collected. Comparison of Smells between patients with infectious disease and noninfectious diseased was performed.
Results
Majority of the participants had no smell. There was no specific odour from infected patients. Among patients with smell, prolonged duration of illness and non-infected people had pleasant odours. Among infected patients, those on antipyretics seem to have more agreeable odours. There was no relation to the type of infection, temperature, respiratory rate, number of medications, or severity of illness with the smells emanating from the patients.
Conclusions
Physician detectable smell is present only in some people. There is no particular ‘infection odour’. A pleasant smell from an infected patient may signify a longer duration of infection.
Keywords
Body Odour, Case control study, Cross sectional study, Infectious disease, Smell, Smell of infection, Smell olfaction
Introduction
Although a physician is confronted with many types of sufferers, patients with infectious disease constitute a significant portion of a clinician’s day to day practice. These patients present with a variety of symptoms and signs. In seeking for the clues for the diagnosis, the practitioner observes, listens and sometimes smells for particular patterns. Anecdotally, it is quite common to smell the putrid odour in diphtheria, the baked bread smell of typhoid [1] and the foul smell of anaerobic infection. The Ancient Indian Sage Sushruta [2] says “by the sense of smell we can recognise the peculiar perspiration of many diseases, which has an important bearing on their identification”.
People infected with vector borne disease like malaria produce odours attractive to mosquitoes [3]. Women can detect aversive odours from nongenital areas of men infected with gonorrhoea [4]. Each of these characteristic odours have plausible biochemical basis, emanating from particular metabolites escaping through the lungs or skin.
Infections are known to cause release of a multitude of chemicals into the blood stream. These chemical mediators called cytokines produce the fever response seen in infectious diseases.IL-1, TNF-α, IL-6, and IFN are the chief pyrogenic cytokines [5], which are produced in response to bacterial endotoxins. Recent experiments involving injection of the endotoxin- Lipopolysaccharide have induced aversive odours from the subjects [6]. An ‘infection odour’ therefore exists. Clinicians come to a provisional diagnosis of infection based on symptoms such as fever, tachycardia and increased leukocyte count. But a characteristic smell of infection has not been described. Moreover, in certain conditions like immunosuppressive state, patients of extremes of age groups and with hypothalamic damage, body temperature does not rise. More over studies have shown that significant number of patients with culture proven infection may not show abnormal temperature or altered leukocyte count [7]. In these cases the detection of an infection specific odour might be useful in detecting the sickness of the patient. We searched for this ‘infection odour’.
Human beings select their life partners based on the scent of their mates [8] and they are also superior to the best technology in sniffing the flavour of quality wines. Hence we used the physician’s nose to detect this ‘infection odour’.
Materials and Methods
Over the month of October 2014, a cross sectional observational controlled study was performed at the Govt. general hospital, Guntur. The research physician approached 52 hospitalised patients admitted for and diagnosed with an infectious disease at the bedside and 61 individuals not using any medication presenting to our tertiary referral hospital for a non-infectious complaint and noted the smell emanating [Although if the chemicals were to escape the blood, they might easily do so from the large alveolar interface of the lung, smelling the nose and mouth for respiratory emissions had disadvantages: Patient had to be able to open the mouth. Deep sniffing from these orifices exposes the physician to potential pathogens. Even with mouth open smell takes significant time to reach physician unless it is very pungent or potent. Hence we did not concentrate on specific sites like mouth and nose]. The interaction lasted for approximately 15 min per patient with measurement of pulse rate for one full minute, axillary temperature for one full minute, and respiratory rate for one full minute, oxygenation by pulse oximetry using a Nellcor N-200(Nellcor Inc, Hayward, CA) co-oximeter finger probe in a sitting position and blood pressure using a Elko Mercury BP apparatus (Elko Inc, Mumbai, India). The same physician interacted with all the subjects. The PIRO [9] system was used to classify the severity of illness.
Statistics
Parametric data is represented with mean and standard deviation. Odds ratio was calculated to compare proportion of smell and no smell in patients and controls. Chi square test was used for categorical variables using Microsoft Excel 2007.
Written informed consent was obtained from all the participants. The study was approved by the Institutional Ethical Committee of Guntur Medical College, India.
Results
The demographic profile of the participants is depicted in Table 1
| Characteristic | Patients[N=52] | Control Persons[N=61] |
|---|---|---|
| Age | 43(2) | 49(2) |
| Female | 34 | 28 |
| Occupation | - | - |
| labourer | 25 | 14 |
| home maker | 17 | 17 |
| unemployed | 5 | 9 |
| baker | - | 1 |
| doctor | - | 3 |
| desk job | - | 2 |
| farmer | - | 11 |
| student | - | 1 |
| semi labour | - | 5 |
| Smell | 16 | 10 |
| No Smell | 37 | 51 |
Table 1: Demographic profile of the participants.
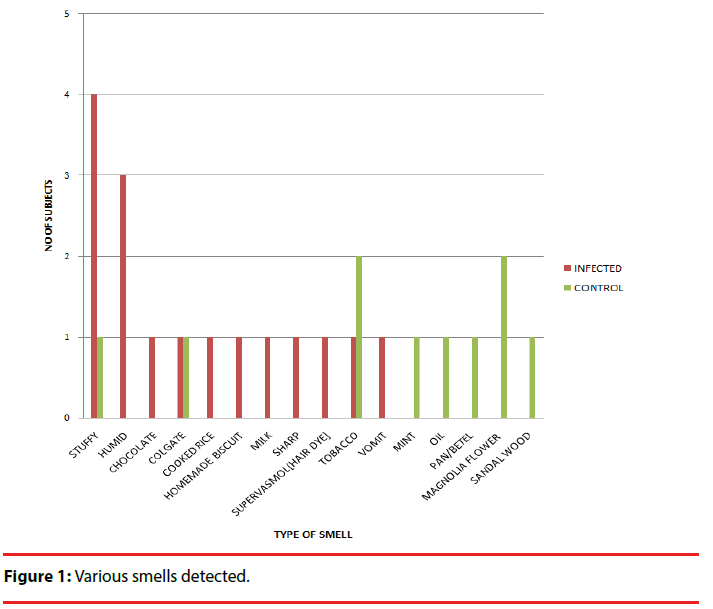
Patients with infection were found have similar proportion of any type of smell when compared to control population [16/53 vs 10/61, OR=2·2(0·9-5·4), p=0·07]. The different smells detected varied in both cases and controls.
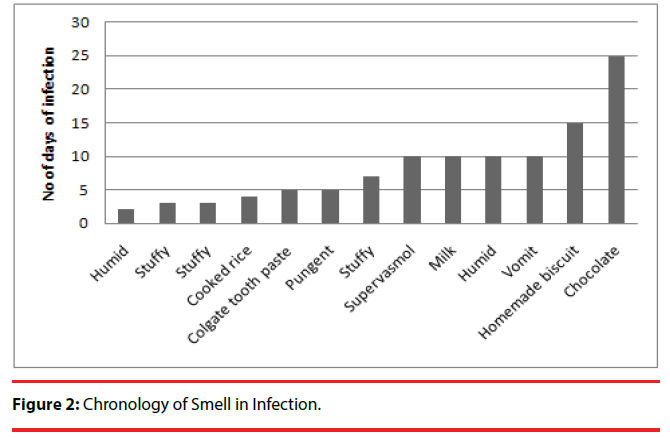
As can be seen in Figure 1 fragrant smells such as mint, magnolia, and sandal wood were more common in controls than in patients [Χ2=7·6, p=0·02]. A peculiar trend of irksome smell to rather agreeable one appears to be seen as the duration of infection increases (Figure 2).
There was no relation to the type of infection (Table 2), temperature, respiratory rate, number of medications or the PIRO stage of the patient with the smells emanating from the infected people.
| Diagnosis | No Of Patients | Smell |
|---|---|---|
| Viral Fever | 6 | No Smell[4], Humid[1], Milk[1] |
| Malaria | 5 | No Smell |
| Urinary Tract Infection | 4 | Stuffy[2], No Smell[2] |
| Hiv | 4 | No Smell[3], Home Made Biscuit[1] |
| Pneumonia | 3 | No Smell |
| Gastroenteritis | 2 | Humid, Sharp |
| Cellulitis | 2 | Cooked Rice, No Smell |
| Meningitis | 2 | No Smell |
| Cerebral Malaria | 2 | Tobacco, Vomit |
| Sepsis | 2 | No Smell |
| Cholecystitis | 1 | No Smell |
| Hepatitis B | 1 | No Smell |
| Pulmonary Tuberculosis | 1 | No Smell |
| Pyelonephritis | 1 | No Smell |
| Tb Meningitis | 1 | Chocolate |
| Viral Encephalitis | 1 | No Smell |
| Unclassified Infection | 14 | No Smell[9],Stuffy[2],Humid[1],Supervasmol[1]Colgate[1] |
HUMID=felt like moisture in the air near a river/sea. STUFFY=like old cloth store rooms.
SHARP=pungent.
Table 2: Odour in different infectious diseases.
Discussion
Both animals and humans have been studied for their ability to detect infectious odours. With only 1/100th capability of a dog, the human nose is far inferior to the canine, but the practical limitations of a sniffing dog in a clinic or hospital seem to restrict the job to the nose of the physician [10,11]. Hence we studied human detection of smell from infected patients. Our study aimed to detect a previously untested hypothesis of smell that may be common to almost all infections. We identified no such specific odour. Although a very small number, stuffy/humid vapours [3/4 patients vs. 1 control] were detected at the infected patient bedside. This may be due to the stagnant air surrounding the patients or due to constant fluid intake, IV fluid therapy, cold sponging or the sweat from the patient punctuating the fever response of the body.
As anticipated, non-infectious diseased people smelled better. They had no infection agent to potentially produce an odour and most of them were more socially active [as infections are considered contagious], necessating in maintaining a pleasing aura around themselves.
We found however those patients with infection over protracted periods tend to have more agreeable odours than those in the acute period. Human beings being social animals automatically tend to appear with pleasant smell in order not to be shunned or alienated by their society [12]. No wonder Sherlock Holmes [13], guessed the solitary victim by the halitosis of his Hat! In any infection, the stress may disrupt this tendency for self-preening. And hence their might be unpleasant smells from the infected patient in early period. As the duration increases, the patient settles into a new equilibrium and the initial stress itself might subside over time in the hospital environment.
In India, many patients are barred from bathing during fever. And the patient is brought to the hospital in such an unwashed state. In the hospital, the care givers are advised and encouraged to clean the patient regularly and in some conditions the staff tend to his cleanliness. This might therefore decrease any disagreeable odour from the patient as his duration of stay increases.
In general the more the duration of illness the more antibiotics are used on the patient, and thus the odour from microorganisms may be lesser in patients who stay longer. It may be plausible that patients with malodour are discharged earlier than their perfumed peers. A ‘smelly’ person is often avoided by most people. Medical personnel are also subject to the same human behaviours.
The use of antipyretics which target the pyrogenic cytokines might influence the odour of the patients, sub group analysis of the infected patients showed an inclination toward stuffy/ humid smell from patients not on antipyretics (Table 3).
| Smell | Antipyretic | No Antipyretic |
|---|---|---|
| Stuffy | 0 | 3 |
| Humid | 2 | 1 |
| Chocolate | 1 | 0 |
| Colgate | 0 | 1 |
| Cooked Rice | 0 | 1 |
| Homemade Biscuit | 0 | 0 |
| Milk | 1 | 0 |
| Sharp | 0 | 1 |
| Supervasmol | 1 | 0 |
| Tobacco | 0 | 1 |
| Vomit | 1 | 0 |
| Any Smell | 6 | 10 |
| No Smell | 21 | 25 |
Table 3: Smell and Antipyretic usage in infected patients.
The pyrogenic cytokines may have produced this discrepancy or they might have altered the patients’ behaviour to consume more fluids and thus contribute to this smell of humidity. Animals in stress emit characteristic odours [14]. The human body also has similar mechanisms [15]. Hospitalisation is a stress by itself and so we matched this potential confounder by hospitalised non-infectious diseased patients as controls. Bias in results due to open label nature of study is minimal as there was no expectation of any particular smell of infection due to lack of previous data. Antibiotics may affect the production of cytokines; their effect could not be assessed in our study as 49 out of 51 infected patients were on antimicrobial treatment, so there was no control for this cohort. Changes in environmental temperature alter the perception of smell [16], this may have affected our study. The subjects were on different types of medication, the effect of which on the results could not be ascertained by the study design.
Studies[11] based on animals and electronic noses have shown good results in detecting various odours to infections, our study may be limited by the comparatively weaker human olfactory apparatus. But physician sniffing the disease is more practical and easy in the real life scenario than to train animals [17] and to leave them onto patients. Similarly electronic noses are quite expensive and are restricted to detect only some volatile substances [11].
In summary, infection in the body per se did not have any human detectable odour. Non infected people tend to smell better due to their self-grooming and possible undercurrent social necessity. Odours emanating from infected patients transform over time to agreeable smells as the acute stress subsides and a new equilibrium is reached. It may also be due to antibiotic related odoriferous microorganism death or medical personnel bias. Temperature of the patient, number of medications or the severity of illness does not significantly change the odour of the infected patient.
Acknowledgment
We are indebted to Dr G Ramakrishna, Assistant Professor of Neurology, Guntur Medical College for internal peer review. We thank Dr Narayana Rao, Specialist Medical Officer, ESI Hospital, Vijayawada for critical external peer review.
References
- Liddell K.Smell as a diagnostic marker. Postgrad. Med. J52(605),136-138(1976).
- Keele KD. The evolution of clinical methods in medicine. Thomas (1963).
- Lacroix R, Mukabana WR, Gouagna LC, et al.Malaria infection increases attractiveness of humans to mosquitoes. PLoS.Biol3(9),e298 (2005).
- Moshkin M, Litvinova N, Litvinova EA, et al.Scent recognition of infected status in humans. J.Sex.Med 9(12),3211-3218(2012).
- Mackowiak PA, Bartlett JG, Borden EC, et al. Concepts of fever: recent advances and lingering dogma. Clin. Infect. Dis25(1),119-138 (1997).
- Olsson MJ, Lundström JN, Kimball BA, et al. The scent of disease: human body odour contains an early chemosensory cue of sickness. Psychol. Sci. Mar25(3),817-823 (2014).
- Seigel TA, Cocchi MN, Salciccioli J, et al. Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J. Emerg. Med 42(3),254-259 (2012).
- Wedekind C, Füri S. Body odour preferences in men and women: do they aim for specific MHC combinations or simply heterozygosity? Proc. R. Soc. B. Biol.Sci264(1387),1471-1479 (1997).
- Chen YX, Li CS. Risk stratification and prognostic performance of the predisposition, infection, response, and organ dysfunction (PIRO) scoring system in septic patients in the emergency department: a cohort study. Crit. Care 18(2),R74 (2014).
- Waggoner LP, Jones MH, Williams M, et al. Effects of extraneous odours on canine detection. 355-362 (1998).
- Bijland LR, Bomers MK, Smulders YM. Smelling the diagnosis: a review on the use of scent in diagnosing disease. Neth. J. Med71(6),300-307 (2013).
- Sarafoleanu C, Mella C, Georgescu M, et al. The importance of the olfactory sense in the human behavior and evolution. J. Med. Life 2(2),196-198 (2009).
- Sherlock Holmes (Character) IMDb. [cited 2015 May 10] (2015).
- Snoddy AM, Heckathorn D, Tessel RE. Cold-restraint stress and urinary endogenous beta-phenylethylamine excretion in rats. Pharmacol.Biochem.Behav.22(3),497-500 (1985).
- Shirasu M, Touhara K. The scent of disease: volatile organic compounds of the human body related to disease and disorder. J. Biochem150(3),257-266 (2011).
- Martin F, Riveron J, Alcorta E. Environmental temperature modulates olfactory reception in Drosophila melanogaster. J. Insect.Physiol57(12),1631-1642 (2011).
- Mahoney AM, Weetjens BJ, Cox C, et al. Using giant African pouched rats to detect tuberculosis in human sputum samples: 2010 findings. Pan. Afr. Med. J9(18),28(2011).