Interest of natural rootsâ≢ exploitation in the optimization of the prosthetic balance: case series
- Corresponding Author:
- Ines Saadellaouiv, DDS, Resident Dentist, Removable Prosthetics Department, ABCDF Laboratory, Faculty of Dental Medicine, University of Monastir, Tunisia
E-mail: saadellaouiines5@gmail.com
Received: 18-September-2023, Manuscript No. ijocs-23-114113; Editor assigned: 19-September-2023, PreQC No. ijocs-23-114113 (PQ); Reviewed: 28-December-2023, QC No. ijocs-23-114113 (Q); Revised: 30- March-2024, Manuscript No. ijocs-23-114113 (R); Published: 03-April-2024, DOI: 10.37532/1753-0431.2024.18 (4).326
Abstract
The conservation of residual roots, when their intrinsic and extrinsic values allow it, and their use as supports of additional means of retention greatly improve prosthetic balance. However, this therapeutic option requires a rigorous implementation and a correct choice of the retention systems better suited to the clinical situation.
This paper aims to present, through two clinical cases, interests of natural roots’ exploitation in the treatment of a large edentulous ridge and to describe the implementation of the axial attachment device.
Keywords
Axial attachment, natural roots, combined prosthesis, conjunction bar
Introduction
The design of a removable partial denture is subordinated to the principles of prosthetic balance. These principles are dictated by the edentulism topography, so it is important to analyze the distribution of the abutment teeth and the rotation axis. In case of a large edentulous ridge bordered by anterior teeth, biomechanical and esthetic problems must be solved. In fact, the difference of compressibility between mucosa and teeth generates rocking motions responsible of patients’ discomfort [1]. Due to the low periodontal value of the anterior teeth, it is not possible to perform retention on them. The treatment of this tooth loss most often requires the use of secondary means of stabilization such as the exploitation of residual roots.
The use of a supra-radicular device can be of great help both functionally and esthetically. It can be used to substitute the vestibular arm of the anterior clasps and to distalize the soft tissue mask. Using residual roots as support has various advantages. It preserves the alveolar bone, maintains periodontal proprioception and increases prosthetic balance [1, 2].
Several conditions must be met so that these residual roots can be preserved citing a healthy periodontal support and a favorable endodontic condition. Different devices can be used to explore these pillars such as attachments and parabolic screed. The aims of this paper were to present, through case series, the interests of natural roots’ exploitation in the treatment of a large edentulous ridge using an axial attachment.
Clinical Case 1
■Patient information
A fifty-two-year-old female patient comes in consultation in the prosthetic department in the university dental clinic of Monastir, Tunisia with functional and esthetic requests.
■Clinical findings
In the maxillary arch, the missing teeth were 22, 24, 25, 26 and 28. Vestibular inlays crowns from 12 to 18 have acceptable aesthetic with a hermetic prosthetic joint. The 23 was a dilapidated tooth.
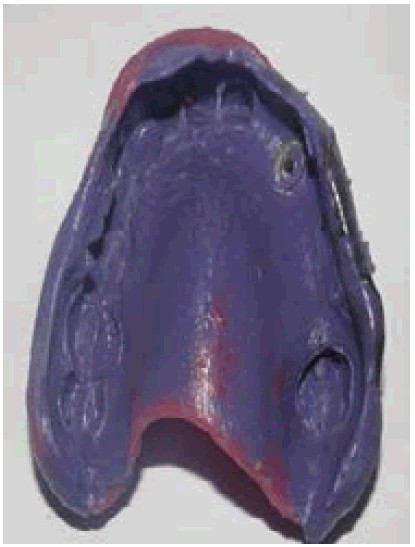
In the mandibular arch, the 46 was the only missing tooth (Figure 1). The examination of the bone mucosa support surfaces revealed a firm and adherent fibro mucosa without any undercuts and a large alveolar residual ridge.
■Diagnostic assessment
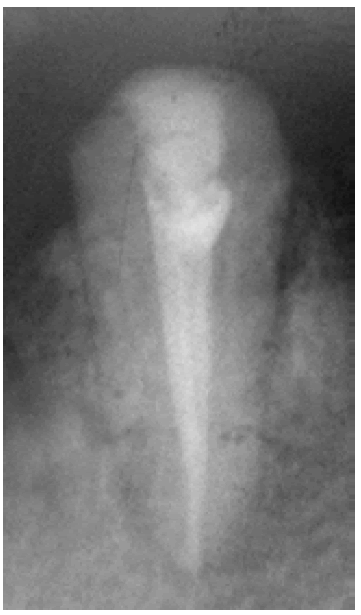
The radiological examination revealed a radiological crown radiological root ratio less than 1 for all teeth. The root canal filling of the 23 was judged hermetic (Figure 2). Study casts’ analysis revealed a sufficient prosthetic usable occlusal height (Figure 3).
Basing on the clinical data and additional diagnostic elements, the prosthetic decision adopted was as follows:
A metallic framework Removable Partial Denture (RPD) with supra radicular attachment (23) was indicated. An axial device was chosen to be connected with the left canine residual root (Rhein 83®). The axial attachment finds all its indications at the 23 since it is an isolated tooth between two edentulous segments with a favorable periodontal factor. In addition, the vertical prosthetic space allows the placement of such device.
There are a wide variety of axial intra radicular attachments, which can be classified into two groups according to the type of movements they allow:
• Rigid attachments, which do not allow any movement other than insertion and disinsertion. All of the forces received by the RPD are transmitted to the tooth carrying the axial attachment.
• Hinged link attachments, which allow a non-rigid connection. The shape of the matrix leaves a space around the Patrice reducing the constraints on the residual roots by involving the fibro mucosa in the prosthetic support [3].
The used rigid attachment presents two parts female and male. The female part incorporates two components: a plastic sheath and a steel case.
The adequate insertion axis was determined after analyzing the study casts on the dental surveyor. This axis will be used for the attachment placement.
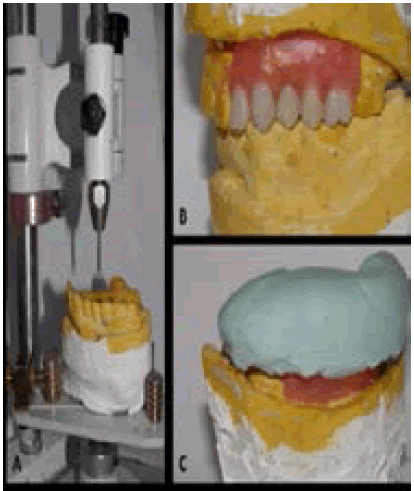
Before starting prosthetic procedures, the prosthetic project was simulated with wax. This simulation facilitates the explanation of the therapeutic plan to the patient in order to obtain her consent. A key with high viscosity silicon was made to visualize the available prosthetic space (Figure 4 A, B, C).
Therapeutic Interventions
■ Preparation of the residual root (23)
To receive the axial device, the residual root of the 23 should be prepared. The occlusal preparation of the cervical plate followed the gingival scallop profile. A chamfer peripheral preparation was done. Two-thirds of the root height were prepared to receive the radicular anchorage. A minimum of 3 mm to 5 mm of the apical sealing should be maintained. The occlusal design of the cervical plate was prepared according to Richmond recommendations’: the buccal wall is beveled while the palatal wall is straight. The buccal wall has a notch, which prevents the rotation of the cope (Figure 5).
■Global impression
An impression was made using a commercial tray with high and low viscosity silicon according to the simultaneous double mixing technique (Figure 6).
■Occlusion registration
The patient occlusion was recorded at centric relation and a correct Occlusion Vertical Dimension (OVD).
■Attachment fixation
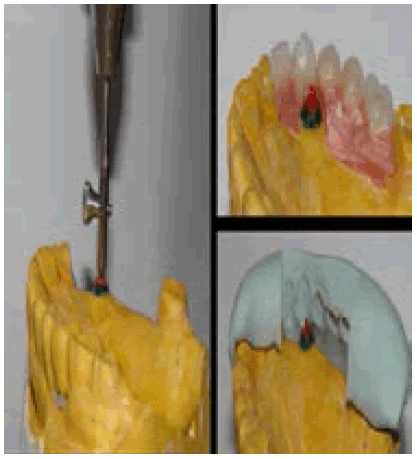
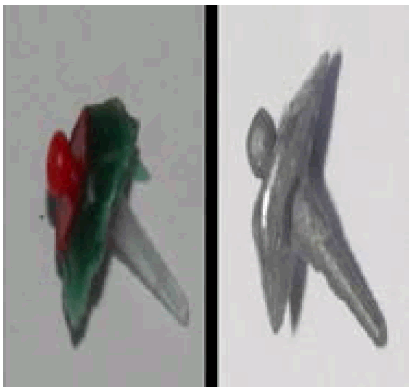
In the laboratory, the fixing of the male part on sub-root coping was made using the dental surveyor with specified instruments. At this point it is easy to control the available prosthetic space using the fabricated silicon key (Figure 7). The obtained wax model was set into the cylinder, then we proceed to the casting (Figure 8). The coping fitted with attachment was validated in the mouth (Figure 9).
■Final impression
A full impression of the bone mucosa support surfaces using an individual tray and poly ether was realized. Consequently, the coping fitted with attachment is integrated in the impression (Figure 10).
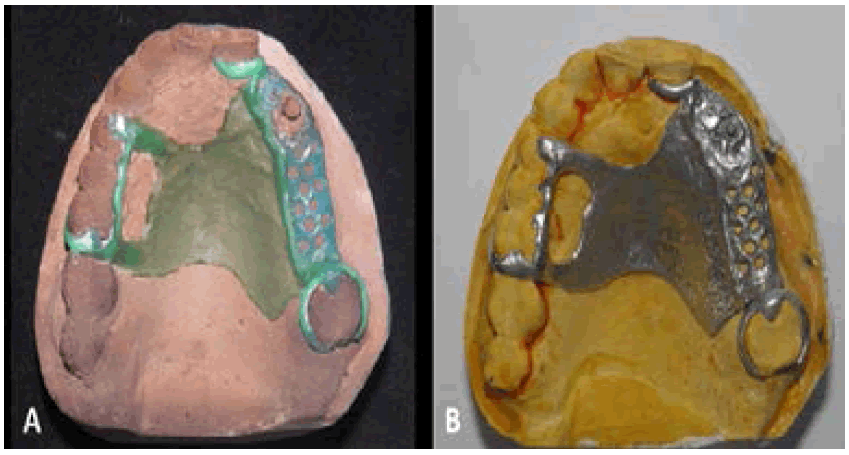
■The realization of the metallic framework RPD
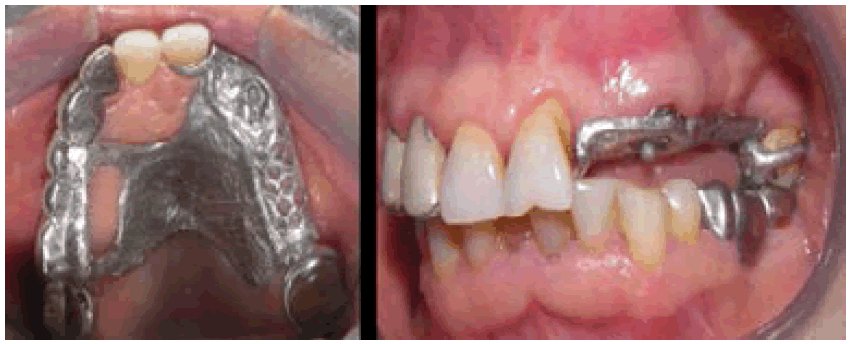
In the laboratory, the metallic framework removable partial denture is realized in different steps (Figure 11 A and B). After that, it is validated in mouth and the jaw relationship at centric relation- OVD correct is recorded (Figure 12). The color of the artificial teeth is chosen and a tooth mounting on wax is realized.
The resin of the removable prosthesis was cured. The coping fitted with axial attachment is sealed on dental root (Figure 13). After that, the intrados of the RPD is recessed in front of the attachment. Occlusion was controlled and equilibration was carried out.
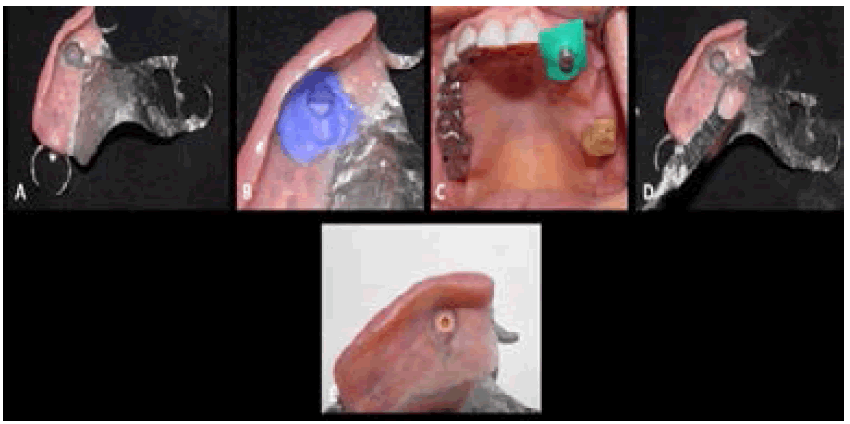
The female part of the axial attachment is integrated in the prosthetic intrados using chemical curing resin under occlusal pressure (Figure 14 A, B, C, D, and E).
Figure 14: The incorporation of the female part of the axial attachment into the maxillary RPD intrados: A: Recessing the intrados of the RPD in front of the attachment; B: Control of the space reserved for the female part; C: Placing the female part of the axial attachment; D: Putting the resin into the RPD intrados; E: RPD with the female part of the axial attachment.
■Follow up and outcomes
The RPD was esthetically and functionally well integrated and the patient was very satisfied with the final result (Figure 15).
Hygiene and maintenance advices were provided to the patient, emphasizing the importance of regular monitoring to sustain the obtained results.
Clinical case 2
■Patient information
A 60-year-old patient, in good general health, consults the prosthetic department for aesthetic and functional prosthetic rehabilitation.
■Clinical findings
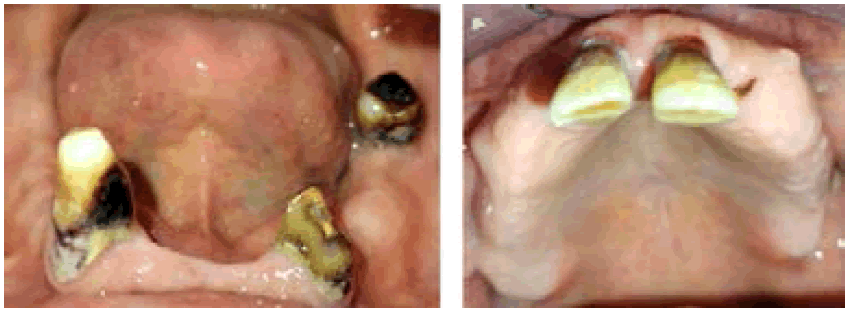
In the maxillary arch, only the two central incisors remain, which were mobile and splintered. The edentulous ridge is high and wide covered with adherent fibro mucosa.
The tuberosities were well formed, the paratuberosity pockets were deep and wide. The palate is wide and deep.
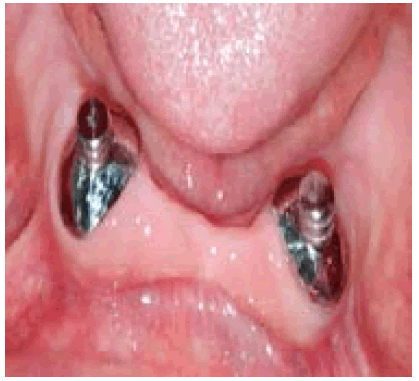
In the mandibular arch, the present teeth were 33, 43 and 37. The 37 was mobile and decayed. There was no mobility in the canines. The anterior crest is straight. In the lateral sectors, it is wide and moderately high covered with adherent fibromucosa (Figure 16).
■Diagnostic assessment
The radiological crown radiological root ratio was equal to 1 for the two canines. The root canal filling of the 33 was judged insufficient.
■Therapeutic interventions
The oral cavity sanitation was done. The 11, 21 and 37 were extracted. The endodontic treatment of the 33 and 43 was done. In the maxillary arch, a removable complete denture was indicated.
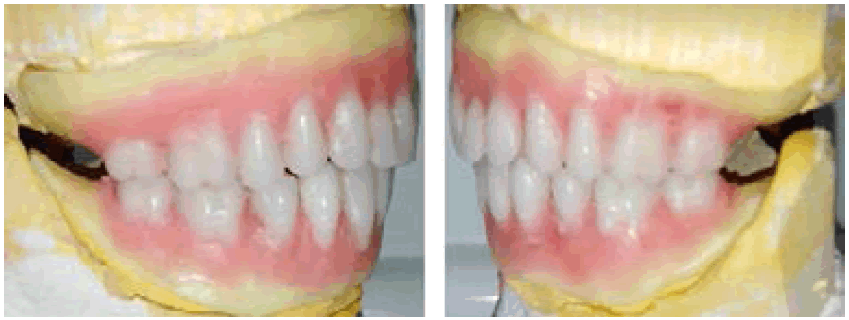
In the mandibular arch, an overdenture complete prosthesis was indicated: two supra radicular attachments (33 and 43) were indicated. Axial devices were chosen to be connected with the two canines’ residual roots (Rhein 83®). Before starting prosthetic procedures, the prosthetic project was simulated with wax (Figure 17).
Keys with high viscosity silicon were made to visualize the available prosthetic space (Figure 18).
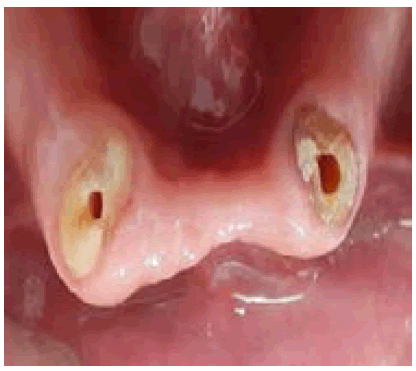
Preparation of the residual roots (33 and 43). To receive the axial devices, the residual roots of the 33 and 43 should be prepared according to Richmond recommendations (Figure 19).
■Global impressions
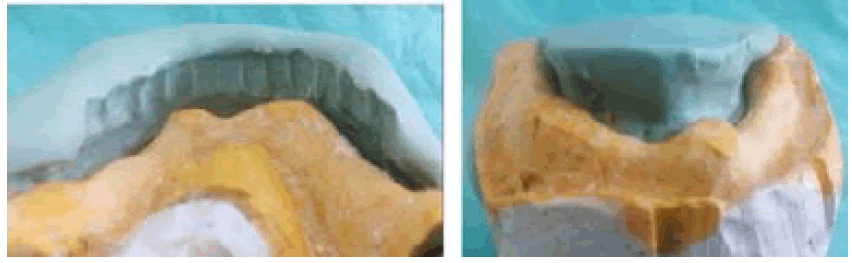
In the mandibular arch, an impression was made using a commercial tray with high and low viscosity silicon according to the simultaneous double mixing technique. In the maxillary arch, the impression was made using an individual tray (Figure 20).
■Occlusion registration
The patient occlusion was recorded at centric relation and a correct Occlusion Vertical Dimension (OVD).
■Attachment fixation
In the laboratory, the fixing of the male parts on sub-roots copings was made using the dental surveyor. The available prosthetic space was controlled using the fabricated silicon keys (Figure 21). The obtained wax models were set into the cylinder, then we proceed to the casting. The copings fitted with attachments were validated in the mouth (Figure 22).
■Final impression
A full impression of the bone mucosa support surfaces using an individual tray and poly ether was realized. Consequently, the copings fitted with attachments are integrated in the impression (Figure 23).
■Occlusion registration
The patient occlusion was recorded at centric relation and a correct Occlusion Vertical Dimension (OVD).
In the laboratory, the mounting of false teeth on wax was realized (Figure 24). Then, prosthetic models were validated in the mouth.
■The realization of the removable complete dentures
The resin of the removable complete prosthesis was cured. The copings fitted with axial attachments were sealed on dental roots (Figure 25). After that, the intrados of the complete dentures is recessed in front of the attachments. Occlusion was controlled and equilibration was carried out.
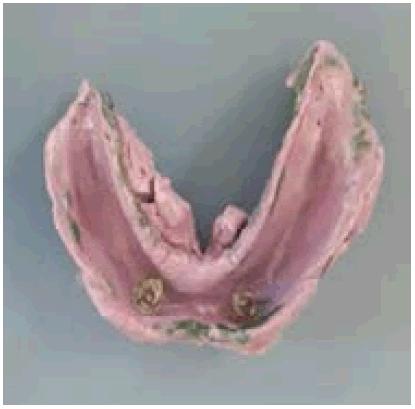
The female parts of the axial attachments were integrated in the prosthetic intrados using chemical curing resin under occlusal pressure (Figure 26).
Figure 26: The incorporation of the female parts of the axial attachments into the mandibular complete denture intrados: A: Control of the space reserved for the female parts; B: Placing the female parts of the axial attachments; C: Putting the resin into the complete denture intrados; D: Complete denture with the female parts of the axial attachments
■Follow up and outcomes
The removable complete dentures were well integrated in the mouth (Figure 27). The patient is currently under surveillance with a follow-up of 7 months.
Discussion
The indication of natural roots conservation must be the result of a preliminary study to justify the prosthetic choice. The most important criteria of choice, which guide us towards the conservation or the extraction of the residual roots are: a healthy periodontal support; a hermetic root canal filling; a sufficient amount of alveolar bone around the root and a good situation of the root on the arch.
Other advantages of root exploitation remain on the reduction of the lever arm, the reduction of the extent of the edentulism and the distalization of the false gum.
The use of the axial attachment in the rehabilitation of a large edentulous ridge is a powerful technique reconciling function, aesthetics and biomechanical balance. Thanks to their design, axial attachments provide a mechanic connection type push button, which guarantees the retention of the removable partial prosthesis on residual roots prepared for this effect. The retention is achieved by friction between the male and female parts of the attachment that is masked by the removable prosthesis. This device prevents the visibility of the vestibular arm of the anterior clasps [3].
The success of the attachment’s implementation is based on different points:
The evaluation of the available prosthetic space and the choice of the attachment’s volume; the prosthetic project simulation and the choice of the adequate insertion axis [1].
In our case, the use of the axial attachment helps to preserve the alveolar bone and the proprioception from a biological point of view. Mechanically, it improves a prosthetic balance. Esthetically, it reduces the clasp’s visibility [4-6].
The criteria which guide us towards the choice between an axial attachment, a conjunction bar and a parabolic screed are the following:
• The available prosthetic space: when this space is sufficient, an axial attachment or a conjunction bar can be indicated, however, when the prosthetic space is insufficient, the parabolic coping can be used.
• The divergence of the roots: when the residual roots are divergent, axial attachments are indicated.
• Root implantation in the bone: a residual root well implanted in the bone can be used as a support for an axial attachment. In the case where the residual roots have an average value of bone implantation, the conjunction bar ensures the restraint of these roots.
• The edentulous crest: if it is straight, the conjunction bar is indicated, otherwise it is curved, and the axial attachment can be used.
The treatment longevity is not just limited to the constraints on attachments, it involves, for the most part, the motivation of the patient and his cooperation, the respect of hygiene rules and periodic check-ups and the integration of the removable prosthesis in the occlusal context of the patient [7].
Conclusion
The extraction of the residual roots should not be systematic, a preliminary study of their intrinsic and extrinsic values as well as their positions on the arch must be carried out. The exploitation of these roots makes it possible to improve or in certain cases to find a balance difficult to achieve. The dentist must keep in mind all the means of exploitation of these roots in order to be able to indicate and implement them.
References
- Saadellaoui I, Mabrouk Y, Mansour L, et al. Interest Of Attachment Use In The Treatment Of A Large Edentulous Ridge: A Clinical Report. Int. Arab J. Dent. 5, 13(2022).
- Triki H, Bekri S, Saddouri I, et al. Treatment of a maxillary edentulism of class V of Kennedy Applegate by composite prosthesis: A case report. R.M.O.S N (2022).
- Bekri S, Triki H, Bibi R, Trabelsi. M. Aesthetic and biomechanical management of a class II Kennedy edentulism case. IAJD. 7, 130-135(2016).
- Fajri L, Hamzaoui S, Berzouk N, et al. Removable partial prosthesis from analysis to realization. AJDI. 19 (2021).
- Bouraoui S, Mansour L, Trabelsi M. et al. Exploitation of natural and artificial roots in removable prosthesis: clinical cases. AJDI. 5, 23-35(2016).
- Sabir S, Slaoui J, Merzouk N, et al. Iintégration d'un attachement axial à une prothèse adjointe partielle métallique: intérêts thérapeutiques. Nord. J. Work. Life Stud. 22, 10 (2020).
- Abdelkoui A, Fajri L, Abdedine A. Racines naturelles et implants au service de l’équilibre prothétique en prothèse amovible complète. Cah de proth. 12, 159(2012).