How to Safely Perform Lumbar Punctures In Adult Patients
- Corresponding Author:
- John A. Emelifeonwu
Department of Neurosurgery
Royal Hospital for Sick Children
9 Sciennes Rd., Edinburgh EH9 1LF, United Kingdom
e-mail: johnemelifeonwu@gmail.com, john_emelifeonwu@hotmail.co.uk
Abstract
The ability to perform clinical skills competently and safely is a big part of being a doctor and as such the General Medical Council (GMC) in its 'Tomorrow's Doctors' document, stresses the importance of acquiring sound clinical skills. Lumbar punctures (LPs) are often considered to be one of the more technically difficult of these clinical skills to perform. This is because performing LPs requires sound anatomical knowledge, safe administration of local anaesthetic and the ability to establish and maintain a sterile field. LPs are used in a wide range of specialties and may be done for diagnostic or therapeutic purposes. Diagnostic LPs include cerebrospinal fluid (CSF) analysis for infection or blood metabolites, whilst therapeutic LPs may be done for example to administer spinal anaesthetic and intra-thecal chemotherapy or to relieve pressure in patients with communicating hydrocephalus. In this article we provide a stepwise overview on how to safely perform an LP.
Keywords
Intra-thecal chemotherapy, Lumbar punctures
Introduction
▪ Starting up
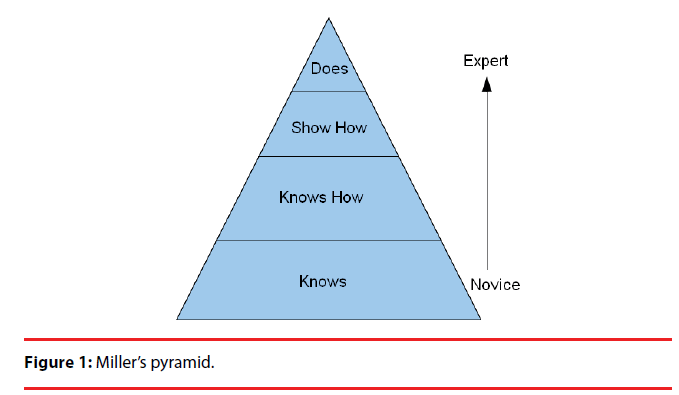
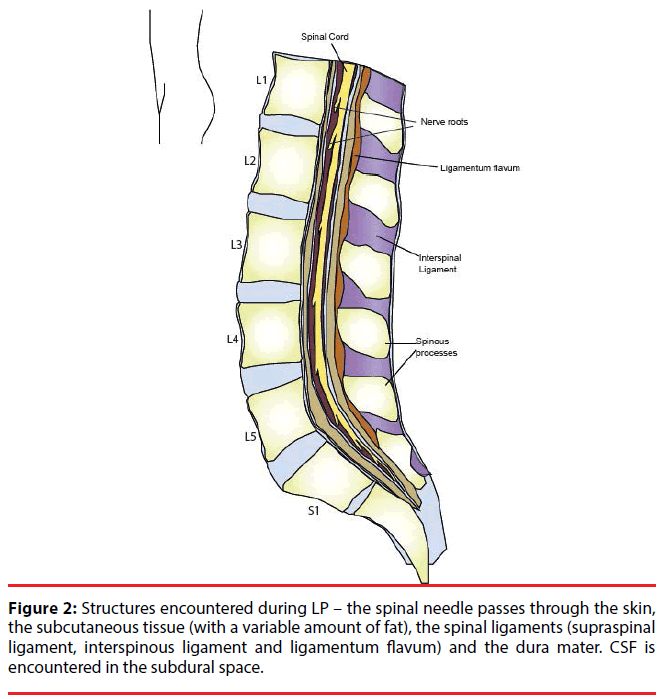
There are currently many theories about how clinical skills should be taught and one of the most widely used is George Miller’s ‘pyramid’ (Figure 1) [1,2]. This describes learning a skill as a hierarchical process during which the learner first learns the theory behind the skill (‘knows’) and is therefore able to explain the necessary steps of the skill to their teacher (‘knows how’). Next the learner must show their teacher that they can perform the procedure (‘shows how’) and in doing so, the learner eventually becomes proficient at performing the procedure (‘does’). Thus, the first stage of learning any practical skill should be to acquire knowledge about the theory behind the procedure. It is therefore important to familiarise yourself with the anatomy of the lumbar spine and the various structures that are encountered during an LP (Figure 2).
Furthermore, it is also important to find out whether the hospital or the Trust in which you work has its own policies and guidelines about how LPs should be performed. Once you are happy that you understand the theory behind how the procedure should be performed, the next step is to get a senior to show you how the procedure is done. We recommend the following steps as safe practice in performing LPs.
▪ Step 1: Assess and consent the patient
Because most doctors now work in shifts, it is often the case that the doctor who clerks the patient may not be the one who performs the LP. Before performing any procedure on any patient, it is essential to perform your own assessment of the patient. Take a history or at least verify the history on the clerking sheet with the patient to confirm the indication. Make sure you know the results of last blood tests – clotting, platelet count. Is patient on any anticoagulants?
Many patients having an LP for acute reasons will first have had a computer-assisted tomography (CT) scan of their head and it is important to review this scan with an appropriate senior colleague or to read the radiology report. Performing LP in a patient with an obstructed or non-communicating hydrocephalus can lead to brain herniation, with potentially disastrous consequences. Suspected raised intracranial pressure (ICP) is a relative contraindication for LP. However, in patients with suspected bacterial meningitis, this practice delays the performance of LP and treatment. When performed after antibiotic administration, it may limit the diagnostic power of CSF analysis. Several studies suggest that high-risk patients can be identified, allowing the majority of patients undergo LP without screening CT [3,4]. Therefore, it is recommended to proceed with LP in patients with suspected bacterial meningitis without a CT scan, unless patients present with one or more risk factors: altered mental state, focal neurological signs, papilledema, seizure within the previous week or impaired cellular immunity [3,4].
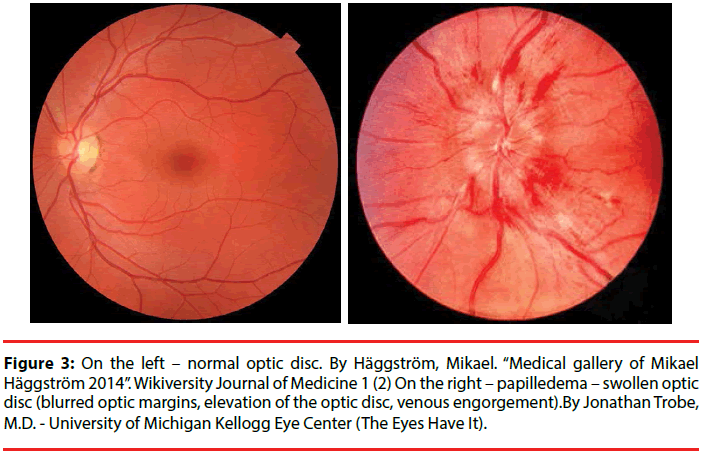
It is also good practice to perform an appropriate clinical examination. We would suggest that all patients should have a lower limb neurological examination before an LP. There is a risk of damage to cauda equina11 nerves during LP, leading to neurological deficits in the lower limb and in such cases it is often useful to have a baseline assessment with which to compare. We would also suggest that fundoscopy should be performed in all patients in whom raised intracranial pressure (ICP) is suspected (Figure 3). It is important to document the results of these examinations appropriately. Finally, the patient should be consented. The current guidelines for consent require the patient to have the capacity to give consent and the doctor to be able to explain the procedure, including the common complications and alternatives to the procedure. Verbal consent is sometimes appropriate, however, some we recommend to get a written consent from your patients with documented patient education. It is therefore important to find out what the practice is where you work. Ensure that you document the consent procedure in the patients’ notes appropriately.
Figure 3: On the left – normal optic disc. By Häggström, Mikael. “Medical gallery of Mikael Häggström 2014”. Wikiversity Journal of Medicine 1 (2) On the right – papilledema – swollen optic disc (blurred optic margins, elevation of the optic disc, venous engorgement).By Jonathan Trobe, M.D. - University of Michigan Kellogg Eye Center (The Eyes Have It).
Contraindications: It is important to note that LPs are contraindicated in certain circumstances.
Absolute contraindications
• Infected skin over the needle entry site and the presence
Increased ICP from any space-occupying lesion (mass or abscess) and trauma or mass to lumbar spine.
• Relative contraindications to LPs include:
• Coagulopathy (high INR, marked thrombocytopenia – ≤ 50 × 109 cells/L) [3].
▪ Step 2: Preparing for the procedure
Some units have ‘Lumbar Puncture packs’, which contain the necessary equipment for performing LPs. These can usually be found in units or wards in which lots of LPs are performed such as the neurosurgery or neurology wards. Failing this, you may find these packs in anaesthetic rooms, especially in theatres where spinal anaesthesia is used commonly. However, there are often cost and other implications when equipment is taken from other units and wards, so do not forget to ask the ward manager and staff before taking any equipment. For LPs the following are required:
Sterile Pack, sterile gloves and skin disinfectant
Because of the risk of inoculating CSF, LPs should be performed using aseptic technique (aseptic hand-wash, sterile gloves, sterile drape and sterile swabs). In immunosuppressed patients and patients in intensive care, the procedure should be performed under sterile conditions i.e. with the performer scrubbed and wearing a sterile gown.
Local anaesthetic: Typically 1% Lignocaine (Lidocaine) is used. The maximum recommended dose is 3mg/kg and most patients require much less than this. Often the most painful part of performing LPs is passing the needle through the well innervated skin. It is therefore important to adequately anaesthetise the skin.
Spinal needle: Several types of spinal needles exist and the type used is often dependent on the indication for LP (Figure 4). The Quincke2 needle allows for direct communication between the subdural space and the manometer, and therefore gives a more accurate measurement of CSF pressure. However, these needles cause more traumatic punctures of the dura unlike pencilpoint needles such as the Sprotte needle. These “atraumatic” needles reduce dural injury and CSF loss and hence reduce the incidence of postdural puncture headache (PDPH). PDPH occurs as a result of intra-cranial hypotension following excess CSF leak and it is also dependent on the size of the spinal needle. Whilst the incidence of PDPH increases with the size of the needle, it is important to note that larger needles (22G or above) allow for better CSF flow and hence are better for measuring CSF pressure [5].
Manometer: Because CSF flow is continuous between the subdural spaces in the brain and the spinal cord, the pressure at which CSF flows at the spinal level is a good indication of intra-cranial pressure and is hence a good diagnostic measure for patients with suspected hydrocephalus. Measuring the pressure before any CSF is withdrawn (‘opening pressure’) is a worthwhile process in most acute situations. Opening pressure should also be measured in all patients with known raised intra-cranial pressure e.g. hydrocephalus, benign intracranial hypertension (BIH) or normal pressure hydrocephalus (NPH). For this group of patients in whom CSF is often withdrawn to relieve symptoms, the pressure should also be measured after CSF is withdrawn (‘closing pressure’) to ensure that the intra-cranial pressure has normalised following the therapeutic LP. Normal CSF pressure in the lumbar region when the patient is horizontal (lateral decubitus) position is 5-15 cm H2O. Opening pressure in patients in the prone (sitting) position can be significantly higher (up to 2-3 cm H2O) [6].
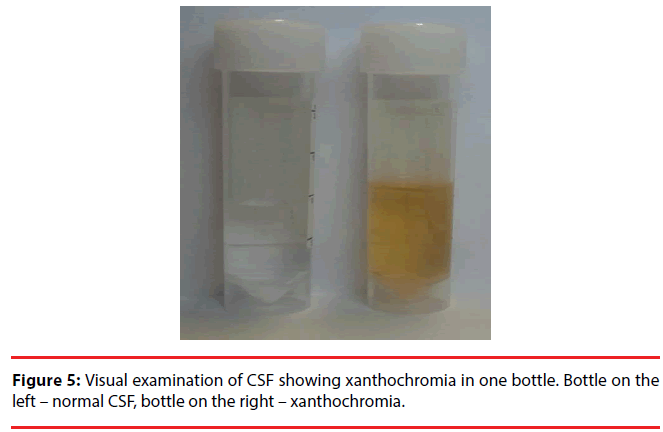
Containers for collecting CSF (diagnostic LPs only): Samples for CSF glucose analysis are usually collected in flouride/oxalate (usually grey-top) vacutainers, whilst samples for analysis of CSF protein, xanthochromia3 and microbiological studies are usually collected in universal containers. Xanthochromia samples need to be protected from light and should be placed in, and transported in an opaque container shortly after collection. It is important to consult with the biochemistry and microbiology departments if you are unsure about how samples should be collected or how to transport samples.
Normal CSF samples should be colourless, clear, like water. The appearance of CSF can be changed due to:
Infectious meningitis – cloudy, milky CSF
Hemorrhage or traumatic tap – xantochromic samples with increased haemoglobin. If CSF samples are centrifuged immediately, xantochromia due to traumatic tap should not occur (Figure 5).
Disorders affecting blood-brain barrier – cloudy samples with increased proteins, albumin and IgG.
Dressing: A suitable dry dressing should be applied to the site of puncture after the procedure.
▪ Step 3: Positioning the patient and anatomical considerations
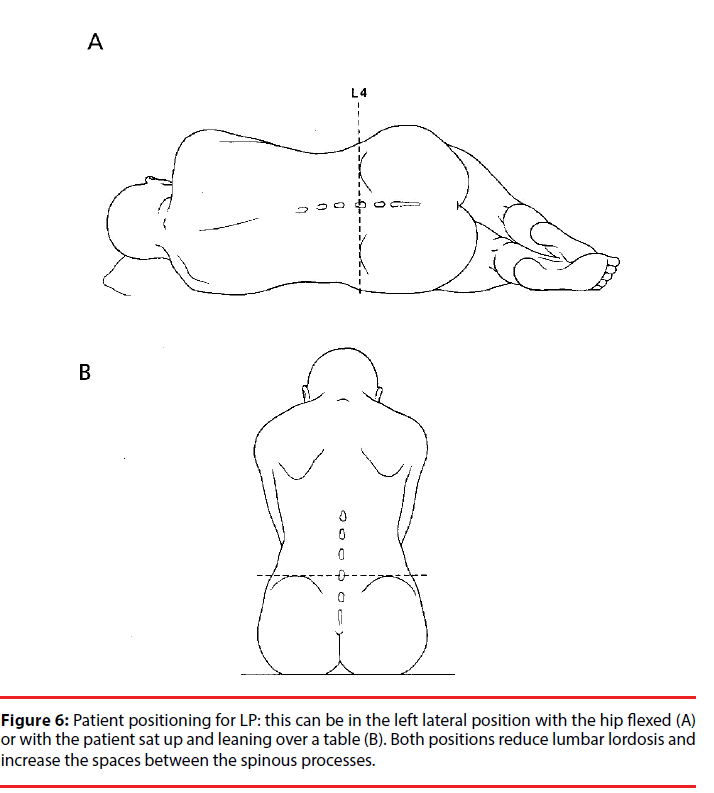
Perhaps the most important step of performing an LP is ensuring optimal patient positioning and being clear where you intend to place your needle. LPs can be performed with the patient in the left lateral position with their knees pulled up to their chest or with the patient sat up and leaning over a table (Figure 6a and 6b). Both allow flexion of the lumbar vertebrae, thus reducing lordosis and increasing the spaces between the lumbar vertebral spinous processes. The left lateral position should be used in all cases that require measurement of CSF pressure.
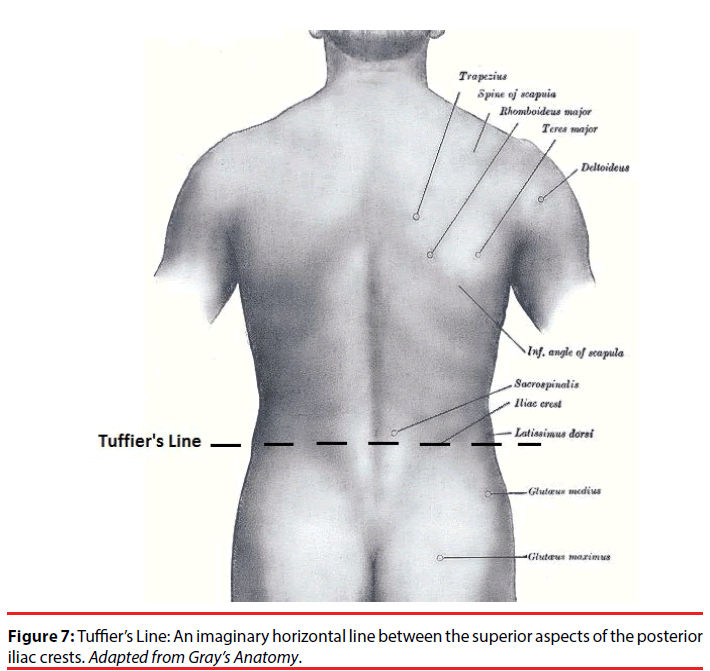
The spinal cord ends at the level of the intervertebral disc between L1 and L2 around 50% of adults, but the range varies from T12 to L3/L4 intervertebral disc [7]. In order to avoid damage to the spinal cord, LPs should be performed below the L3 vertebrae, typically in the L3/L4 or the L4/L5 intervertebral spaces. The most accurate surface anatomy is the intercristal line (Tuffier’s line4), which is an imaginary horizontal line between the superior aspect of the posterior iliac crests (Figure 7). Tuffier’s line crosses the body of L4 in most patients in the left lateral position and the L3/L4 intervertebral space in most patients in the seating position [8].
LPs are performed through a needle puncture in the midline. It is important to remember that the spinal processes project inferiorly. Therefore the needle should be introduced aiming slightly superiorly-aiming towards the umbilicus (approximately 15° cephalad) is usually sufficient to avoid hitting spinal process. Not every patient has a vertebral column in the median axis – ask the patient if he or she feels any pain radiating to the left or right leg – you might need to correct the positioning of the needle more laterally. When you start introducing the needle, ask the patient if he or she feels any pain. Local anaesthetic might need more time to start working.
LPs are performed through a needle puncture in the midline. It is important to remember that the spinal processes project inferiorly. Therefore the needle should be introduced aiming slightly superiorly-aiming towards the umbilicus (approximately 15° cephalad) is usually sufficient to avoid hitting spinal process. Not every patient has a vertebral column in the median axis – ask the patient if he or she feels any pain radiating to the left or right leg – you might need to correct the positioning of the needle more laterally. When you start introducing the needle, ask the patient if he or she feels any pain. Local anaesthetic might need more time to start working.
The structures encountered are skin, subcutaneous tissue (with a varying degree of fat), supraspinous ligaments, interspinous ligaments, the ligamentum flavum5, epidural space, the dura mater and finally the subdural space in which CSF is encountered (Figure 2). There are no muscles crossing the midline. The ligamentum flavum is a tough and elastic fibrous structure that is often a useful landmark for those experienced in performing LPs.
Complications
The most common complication following LP is post-dural puncture headache (PDPH), which can be as high as 70% depending on the type of needle used [9]. The incidence of postdural puncture headache may be reduced with a pencil-point needle. As it is a significant cause of morbidity, it should always be discussed when you are consenting the patient, especially in high-risk patients, such as young women with a low body mass index and during pregnancy [9,10].
The patient should be advised to remain in the horizontal position for up to an hour after the procedure to prevent low pressure headaches, especially when lots of CSF is withdrawn.
More than 80% of PDPH resolve with supportive treatment – rehydration, analgesia and antiemetics. If the headache fails to resolve in 72 hours, then specific treatment is indicated:
Blood patch – 20-30 ml of blood is taken from a vein and injected into the epidural space. It will form a clot and seal the perforation, preventing further leak of CSF.
Other measures: epidural saline – also has a sealing effect; caffeine; surgical closure of the dural gap [9,10].
Other complications include back pain, nerve irritation, bleeding, infection, cranial neuropathies and spinal or cerebral herniation.
Rarely, patients can develop spinal haematoma after LP (especially those with bleeding disorders) – you should think about that if the patient develops neurologic symptoms after LP – leg weakness, decreased sensation or incontinence [11].
In summary, LPs represent one of the more technically challenging bedside clinical skills to perform, however, with sufficient preparation, the right knowledge and appropriate teaching, this useful skill can be performed safely by junior doctors.
References
- Counci GMGood Medical Practice 2014 [cited 2016].
- Miller GE. The assessment of clinical skills/competence/performance. Acad Med65(9 Suppl),S63-67 (1990).
- Joffe AR. Lumbar puncture and brain herniation in acute bacterial meningitis: a review. J Intensive Care Med 22(4),194-207 (2007).
- Gopal AK, Whitehouse JD, Simel DL,et al.159(22)Cranial computed tomography before lumbar puncture.Arch Intern Med ,2681-2875 (1999).
- Anderson M. Choosing the best needle for diagnostic lumbar puncture. J Emerg Med15, 126(1997).
- Schwartz KM, Luetmer PH, Hunt CH,et al., Position-related variability of CSF opening pressure measurements. AJNR Am J Neuroradiol34(4), 904-907(2013).
- Reimann AF and Anson BJ. Vertebral level of termination of the spinal cord with report of a case of sacral cord. Anat Rec88(1), 127-138 (1944).
- Pysyk CL, Persaud D, Bryson GL,et al. Ultrasound assessment of the vertebral level of the palpated intercristal(Tuffier's) line. Can J Anaesth57(1),46-49(2010).
- Turnbull DK. Post-dural puncture headache: pathogenesis, prevention and treatment. 91(5)Br J Anaesth, 718-729(2003).
- Ahmed SV, Jayawarna C, Jude E. Post lumbar puncture headache: diagnosis and management. Postgrad Med J82(973), 713-716(2006).
- Adler MD, Comi AE, Walker AR. Acute hemorrhagic complication of diagnostic lumbar puncture. PediatrEmerg Care17(3),184-188(2001).
- Williams A.Xanthochromia in the Cerebrospinal Fluid. PractNeurol4(3), 174-175 (2004).