How Long Should A Healthcare Practitioner Feel For A Pulse?- A Literature Review
- Corresponding Author:
- Richard Clark
College of Health
Wellbeing and Life Sciences Sheffield Hallam University
Sheffield City United Kingdom
E-mail: R.Clark@shu.ac.uk
Abstract
Assessing the vital signs of a patient is a fundamental technical skill that is routinely performed by healthcare practitioners and can help to indicate whether a patient is at risk of deteriorating. Palpating the peripheral pulse is frequently seen as a simple task when undertaking the assessment of vital signs and, often, little thought may be given to the amount of time which healthcare practitioners attribute to this task. Nursing undergraduate students are regularly taught that a minute is the ideal amount of time that a pulse should be palpated, however in practice this is sometimes reduced to 15 or 30 seconds to save time. This article explores how much time the healthcare practitioner should palpate the pulse to achieve an accurate reading by examining the available literature.
Keywords
Vital signs; Assessing pulse; Palpating pulse.
Introduction
There are many complex reasons for delays in identifying when a patient may be deteriorating. These reasons could include technical skills such as a failure to assess the patient in a timely manner, or non-technical skills such as a breakdown in communication, distractions, poor teamwork, poor decision making, or a loss of situational awareness [1]. It is important to be aware of these reasons to improve patient safety and patient outcomes. Many healthcare organizations have begun to implement stringent systems and interventions such as early rapid response systems aimed at reducing the risk of failing to recognize a deteriorating patient with an aim to begin treatment in a timelier manner [2,3]. This article will look at the importance of assessing vital signs and in particular palpating the pulse and the variations in practice that is evident within the clinical setting.
Other reasons for these delays in recognizing when a patient may be deteriorating could be due to incomplete vital signs assessment or even poor technique when checking vital signs [4]. Checking a patient’s vital signs is a fundamental technical skill that is undertaken by healthcare practitioners to assess whether a patient is haemodynamically stable or at risk of deteriorating [5]. The Resuscitation Council (UK) defines a patient as being ‘haemodynamically stable’ when the patient does not have any difficulties with their circulation, cognitive or respiratory status [6]. Therefore, it is essential to check vital signs as part of a routine physiological assessment to aid the recognition of a deteriorating patient [7]. The Nursing and Midwifery Council is clear that all nurses should accurately assess for signs of normal or worsening physical health in the patient or client that is receiving care [8]. Furthermore, the nurse must immediately refer or escalate to an appropriate professional colleague when it is in the best interests of the individual needing treatment. This suggests that the accurate assessment of vital signs and recognizing when to seek medical support is an essential professional requirement for nurses.
Vital signs can give an early warning in to a wide range of medical problems and also determine how quickly medical interventions are required. For example, vital signs such as a recorded blood pressure can indicate whether the patient is potentially hypovolemic and a high pulse rate may indicate a clinical problem, such as an early indication of sepsis. Indeed, they may indicate many other emergency conditions where early treatment is required.
Recording Vital Signs
“Vital signs” is more commonly referred to as an umbrella term which includes six physiological parameters for assessment. These are; respiration rate, oxygen saturation temperature, systolic blood pressure, heart rate, and level of consciousness. When looked at collectively, they can help generate a picture as to the wellness of the patient. Other vital signs such as urine output, which is a useful indicator of vital organ perfusion (>0.5 ml/kg/hr) and pain score are often assessed if appropriate to do so and if the healthcare practitioner requires them to be monitored [9]. There have been many studies undertaken internationally that would suggest that regular vital signs monitoring will improve patient outcomes and can, in effect, prevent unnecessary deaths [10-12].
The National Early Warning Score (NEWS) was developed in 2012 by the Royal College of Physicians, London, and has since been updated (National Early Warning Score 2, (NEWS2)) with some additional information and to align with the Resuscitation Council’s systematic ABCDE approach [13]. The ABCDE approach is a systematic method of prioritising the assessment of a deteriorating patient. This commences with ‘A’ for airway assessment and concludes with ‘E’ for exposure, which involves a ‘top to toe’ examination of the patient [14].It is an assessment tool designed to aid the healthcare practitioner is not only assessing their patient’s vital signs but also responding to the findings by measuring them to set standardised parameters.
NEWS is based on an aggregate scoring system and can quickly help the clinician determine the degree of deterioration or improvement to the patient’s condition or illness.
NEWS2 was developed in response to various studies which had suggested that a failure across multidisciplinary teams to effectively recognize the signs of deterioration in some patients [15]. By allocating a score to each measurement of six physiological parameters, the healthcare practitioner is able to determine whether a patient is acutely unwell and recognize when to seek support:
• respiratory rate
• oxygen saturation
• temperature
• systolic blood pressure
• heart rate
• level of consciousness (Table 1)
Table 1: Measurement of six physiological parameters.
| Physiological parameter | Score | ||||||
| 3 | 2 | 1 | 0 | 1 | 2 | 3 | |
| Respiration rate (per minute) | ≤ 8 | - | 9-11 | 12-20 | - | 21-24 | 25 |
| SpO2 Scale 1 (%) | ≤ 91 | 92-93 | 94-95 | ≥ 96 | - | - | - |
| SpO2 Scale 2 (%) | ≤ 83 | 84-85 | 86-87 | 88-92 (≥ 93 on air) |
93-94 on oxygen | 95-96 on oxygen | ≥ 97 on oxygen |
| Air or Oxygen? | - | Oxygen | - | Air | - | - | - |
| Systolic Blood Pressure (mmHg) | ≤ 90 | 91-100 | 101-110 | 111-219 | - | - | ≥ 220 |
| Pulse (per minute) | ≤ 40 | - | 41-50 | 51-90 | 91-110 | 111-130 | ≥ 131 |
| Consciousness | - | - | - | Alert | - | CVPU | |
| Temperature (°C) | ≤ 35.0 | - | 35.1-36.0 | 36.1-38.0 | 38.1-39.0 | ≥ 39.1 | - |
Table 2: Filtered relevant papers to check pulse.
Royal College of Physicians (2018)
National Early Warning Score 2 (NEWS2)- Standardising the assessment of acute illness severity in the NHS: NEWS2 is recommended internationally in the routine assessment of all patients over 16 years of age. However, this excludes some patient groups such as pregnant women because the response to illness can be altered and therefore potentially misleading to the clinician. It is worth highlighting that NEWS2 should be used as an aid alongside other clinical considerations. For example, if the NEWS score did not trigger an immediate concern, but other indicators did, such as the patient’s history or presenting condition, then early medical support should still be sought. For example, the ABCDE assessment may still lead to concerns about the patient’s respiratory pattern or circulation, or blood results may be abnormal, even though the NEWS score has not highlighted signs of deterioration as the patient continues to compensate.
Definition of the Pulse
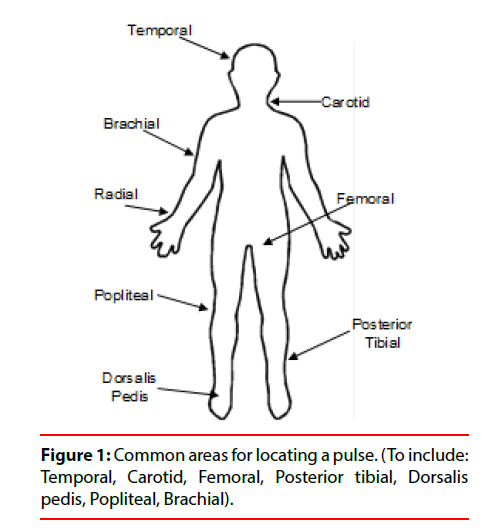
As the left ventricle of the heart contracts, the artery dilates under the increased pressure of contraction [16]. This happens simultaneously all over the body and when this dilation occurs over a non-resistant area such as a bone, a pulse can be felt. Therefore, one pulse is equal to one heartbeat. Within the healthcare setting, healthcare practitioners will more commonly search for a pulse by palpating the radial artery which is located to the right of the wrist as this is usually more easily accessible and is superficial to the patient’s skin [17]. For example, the brachial pulse which can be located in the medial side of the upper arm, or the carotid pulse which is located on either side of the windpipe. Other sites around the body for assessing the pulse can be seen in Figure 1.
However, if the patient is in shock, which can be defined as a state of impaired cellular delivery or utilization of oxygen, the radial pulse, and other peripheral pulses may be less easy to locate or may even be missing. If this is the case and the radial artery isn’t present, other sites such as the carotid artery or the femoral artery sites should be used instead, whereas a bounding pulse may indicate sepsis [18]. There are also variations in pulse rates depending on the patient’s age, coexisting medical conditions, comorbidities, and fluid status [9].
A normal pulse rate in a healthy adult can range from 60 to 80 beats per minute when they are at rest and can reach up to 180 (tachycardia) when excessive stresses such as vigorous exercise are performed [19]. However, a fit person can have a resting heart rate as low as 40 beats per minute (bradycardia) without experiencing any problems. Therefore it is important to consider the pulse within such patient contexts.
⪠Assessing the Pulse
The pulse is a common, yet essential part of assessing the vital signs and should be competently assessed when the healthcare practitioner is completing a NEWS score [20]. When palpitated manually, the pulse offers a great deal of information. Manual palpation of the pulse can not only offer the heart rate but also indicate the strength, amplitude, and regularity of the pulse, which in turn enables the healthcare worker to undertake a bedside assessment of the patient’s cardiovascular status of the heart [21]. Lomas & West argue that using an automated electrical device such as pulse oximetry monitor, for checking the pulse, the healthcare practitioner is more likely to miss these signs and can become less skilled in detecting when a patient is deteriorating (Figure 2) [22].
Palpating the Peripheral Pulse
Although assessing the pulse is seen as a routine procedure, it is not always clear as to how long one should palpate a pulse rate. It has become clear that there is a variation in practice between healthcare practitioners whereas some believed palpating the pulse for one minute was the gold standard whilst others were happy to check for just 30 seconds or even less.
Data was located via CINAHL and Medline searches of peer-reviewed, academic journals, books, reports, documents, and opinion papers, as well as grey literature such as dissertations available via the search engines. Boolean terms such as “and/not/or” were utilised to limit and enhance the search. The inclusion criteria ensured that only full-text data in the English language was located. Due to the lack of literature identified it was essential to search over a broad period of time and therefore 2000 was selected as a starting point. It was necessary to amend the search terms numerous times to increase the number of results generated. Data collection continued until saturation was reached. Saturation was defined as rigorous searching of the literature based on the above search limitations until the concept was exhausted and no new literature was produced. Many papers were excluded as they specifically related to the pulse rate within maternity care or stroke care for example but did not include an evidence base for why the pulse was checked for that time period. Following a review of the results, these were filtered to ensure only relevant papers such as peer reviewed articles or books were used. A total of 15 sources were selected for further analysis and this was then further reduced to nine sources following the filtering process and these are listed below: (Table 2).
| Author | Year | Country | Time to check pulse |
| Richardson | 2008 | UK | 1 minute |
| Hammond R, Spurgeon H | 2015 | UK (Royal Marsden) |
1 minute |
| Jamieson et al. | 2002 | UK | 1 minute |
| Everett, Wright | 2011 | UK | 1 minute |
| Bullock et al. | 2012 | UK | 1 minute |
| Thomas, Monaghan | 2010 | UK (Oxford Handbook) |
1 minute (but could be 15 seconds × 4) |
| Perry et al. | 2012 | UK | 30 seconds × 2 is especially accurate for rapid pulses |
| Andris et al. | 2006 | USA | 30 seconds × 2 |
| Baston | 2001 | UK | 30 seconds × 2 unless irregular then 1 minute |
Discussion
It appears that the main bulk of the literature would recommend that the healthcare practitioner count the number of beats felt within a one minute period and document the findings on the observation chart [23-25]. The rationale for counting for a full minute according to The Royal Marsden Hospital Manual of Clinical Nursing Procedures is that this allows time for the healthcare practitioner to assess for irregularities or defects in the pulse which could, in turn, lead to further complications such as breathlessness and may therefore require further medical investigation [26,27]. However, this rational derives from Rawlings-Anderson & Hunter who state that the pulse should be counted for 60 seconds in the first instance [28]. And subsequent readings may be taken for only 30 seconds and doubled providing that the first reading was of good volume and regular in rhythm.
The Oxford Handbook of Clinical Examination and Practical Skills also agrees that the most accurate method is to count the pulse for a full minute [29]. However, they also suggest it is more common in the clinical setting for the healthcare practitioner to count for only 15 seconds and then multiply by four. This can often be seen as an efficient way in which healthcare staff can save time.
The Nursing Interventions & Clinical Skills book disagrees and states that as long as the pulse is regular in rhythm, the healthcare practitioner may count for 30 seconds and multiply by two [30]. They also go on to state that 30 seconds will give an accurate reading for a ‘regular tachycardia’ (>100 beats per minute) or a ‘regular bradycardia’ (<60 beats per minute) heart rate. However, if the pulse rate is deemed to be irregular in rhythm, then it is recommended that the pulse should be counted for a whole minute. Andris et al. agree with this method, but they do not suggest that the regularity of the pulse should be an indicator when counting for a specific length of time [31]. Instead, it is suggested that counting for 30 seconds is reasonable. However, it was argued that irregular pulses should always be counted for the whole minute [32].
It has also been suggested that counting a pulse for just 30 seconds is especially accurate for ‘rapid’ pulses [33]. Although these varying recommendations are given, there appears to be little offered in terms of evidence or research to back up these claims.
Other publications that were identified did not specify an exact length of time in which the healthcare worker should feel for a pulse. This possibly allows the healthcare practitioner to use anecdotal experiences to determine how they should check a pulse or refer back to when and how they were taught as an undergraduate.
Conclusion
Despite the manual checking of a pulse rate to ascertain beats per minute been a routine clinical procedure and an essential component of a NEWS score calculation, this literature review has concluded that the evidence base is limited. There is a lack of research to support the argument for 15 seconds, 30 seconds, or one minute as the gold standard of clinical practice. The available literature is often contradictory. Following the failure to achieve a suitable rationale for how long a healthcare practitioner should manually palpate a pulse within the available literature, it was decided by the authors that further investigation was required and that research was to be undertaken.
Conflict of Interest
There is no actual or potential conflict of interest in relation to this article.
References
- Clark R. How patient safety zones are improving care quality. The Ergonomist 558, 22-23 (2017).
- McGaughey J, O’Halloran P, Porter S, et al. Early warning systems and rapid response to the deteriorating patient in hospital: A systematic realist review. J Adv Nurs 73, 2877-2891 (2017).
- Tucker G, Lusher A. The use of early warning scores to recognise and respond to patient deterioration in district nursing. Br J Community Nurs 23, 76-79 (2018)
- Stevenson JE, Israelsson J, Nilsson GC, et al. Recording signs of deterioration in acute patients: The documentation of vital signs within electronic health records in patients who suffered in-hospital cardiac arrest. Health Informatics J 22, 21-33 (2016).
- Smith G, Recio-Saucedo A, Griffiths P. The measurement frequency and completeness of vital signs in general hospital wards: An evidence free zone? Int J Nurs Stud 74, A1-A4 (2017).
- Resuscitation Council United Kingdom. Advanced life support. Post-resuscitation care 7th Edition, 153-162 (2017).
- Hands C, Reid E, Meredith P, et al. Patterns in the recording of vital signs and early warning scores: Compliance with a clinical escalation protocol. BMJ Qual Saf 22, 719-726 (2013).
- The Code: Professional standards of practice and behaviour for nurses and midwives associates. Nursing and Midwifery Council, London (2015).
- Elliott M, Coventry A. Critical care: The eight vital signs of patient monitoring. Br J Nurs 21, 621-625 (2012).
- National Institute for Health and Clinical Excellence. Acutely ill patients in Hospital: Recognition of and response to acute illness in adults in hospital. NICE clinical guideline, London (2007).
- National consensus statement: Essential elements for recognising and responding to clinical deterioration. Australian Commission on Safety and Quality in Health Care (2010).
- National Early Warning Score (NEWS): Sandarding the assessment of acute-illness severity in the NHS. Report of a working party. Royal College of Physicians (2012).
- National Early Warning Score 2 (NEWS2): Standardising the assessment of acute-illness severity in the NHS. Royal College of Physicians (2017).
- Smith D, Bowden T. Using the ABCDE approach to assess the deteriorating patient. Nurs Stand 32, 51-61 (2017).
- Day T, Oxton J. The national early warning score in practice: A reflection. Br J Nurs 23, 1036-1040 (2014).
- Patton K, Thibodeau G. Structure & function of the body. Elsevier 15th Edition, 1-306 (2016).
- Waugh A, Grant A. Ross & Wilson: Anatomy & physiology in health & illness. Churchill Livingstone 10th Edition (2006).
- Adam S, Osborne S, Welch J. Critical care nursing: Science and practice. Oxford: Oxford University Press 3rd Edition (2017).
- Rutishauser S. Physiology and anatomy: A basis for nursing and health care, Churchill Livingstone, London. Nurs Stand 9, 1-55 (1997).
- Lowry M, Ashelford S. Assessing the pulse rate in adult patients. Nurs Times 111, 18-20 (2015).
- Lynn P. Clinical Nursing Skills. Wolters Kluwer 4th Edition, 1-55 (2015).
- Lomas C, West D. Skills lost as automation takes over. Nurs Times 105, 1-21 (2009).
- Richardson R. Clinical skills for student nurses: Theory, practice and reflection. Scion Publication 1st Edition, 1-560 (2008).
- Jamieson E, McCall J, Whyte L. Clinical Nursing Practices. Churchill Livingstone 4th Edition (2002).
- Everett F, Wright W. Measuring vital signs: An integrated teaching approach. Nursing Times 107, 16-17 (2011).
- Hammond R, Spurgeon H. The Royal Marsden Hospital manual of clinical nursing procedures. Wiley-Blackwell 9th Edition, 1-603 (2015).
- Bullock I, Clark J, Rycroft-Malone J. Adult nursing practice- Using evidence in care. Oxford University Press (2012).
- Rawlings-Anderson K, Hunter J. Monitoring pulse rate. Nurs Stand 22, 41-43 (2008).
- Thomas J, Monaghan T. Oxford handbook of clinical examination and practical skills. Oxford University Press. Oxford 2nd Edition (2010).
- Perry A, Potter P, Elkin M. Nursing interventions & clinical skills. Elsevier 5th Edition (2012).
- Andries D. Assessment- An incredibly easy! Pocket guide. Lippincott Williams & Wilkins Publication USA 1st Edition (2006).
- Baston H. The practising midwife. Pulse Respiration Measurement. Midwifery basics 4, 1-18 (2001).
- Perry A, Peterson V, Potter P. Basic skills & procedures. Mosby 5th Edition (2003).