Giant Osteochondroma of the Proximal Fibula: A Rare Case
- Corresponding Author:
- Sudhir Shyam Kushwaha
Assistant Professor, Department of Orthopaedics
Era’s Lucknow Medical College, Lucknow, India
Tel: 0522-4153777
Fax: 0522-2407824
E-mail: sudhirshyamkushwaha@gmail.com
Abstract
Osteochondroma is one of the most common benign tumors arising from the ends of the long bones which are characterized by irregular bony growth covered by cartilaginous cap. The tumor mass tends to grow eccentrically more, rather than centrifugally. We are reporting a case of 17 year old female who presented to our Outpatient department with large, hard, painful, irregular swelling over anterolateral aspect of right knee. After a series of radiographic screening and its confirmation through CT the tumor was surgically excised and histopathological reports showed benign nature of the tumor mass excised.
Keywords
Osteochondroma, Proximal fibula, Benign tumor
Introduction
Fibula is not a common location of primary bone tumours. Bone tumours of fibula comprises 2.5% of primary bone lesions [1,2]. The tumours most commonly arising from proximal fibula are Osteochondromas, Giant cell tumours, Osteosarcomas, and Ewing’s sarcoma. Osteochondromas are solitary in 90% cases but they can be sessile or pedunculated also. The tumour mass is usually covered by a cartilaginous cap. Osteochondromas clinically present as painless masses or bony swelling; however, due to their closed vicinity to neurovascular bundles they can also present as compressive neuropathy of peroneal nerve or vascular compression syndrome or a skeletal deformity or pseudoaneurysm of popliteal vessels [3]. Depending upon the growth, surgical treatment option of proximal fibular osteochondroma may vary from debulking of large mass to resection of proximal fibula [4]. In our case the main indication of surgery in form of resection of proximal fibula was cosmetic one and intense pain with associated restricted range of motion in right knee.
Case Description
A 17-year old female presented to our Outpatient department with pain, swelling, and difficulty in walking and deformity in antero-lateral aspect of right proximal leg. Patient was asymptomatic 6 years back when she noticed swelling which was small and painless initially and lateral on progressed with time to an enlarged painful irregular mass. There was no history of trauma, fever or weight loss. Pain was initially dull aching and intermittent and later become continuous and increased on movement.
On examining the patient clinically, a large swelling was present on the anterolateral aspect of proximal part of (R) leg of size about 12 × 11 × 10cm. The swelling had gradually increased from the size of approximately 3 × 4 cm to present size of this in last six years.
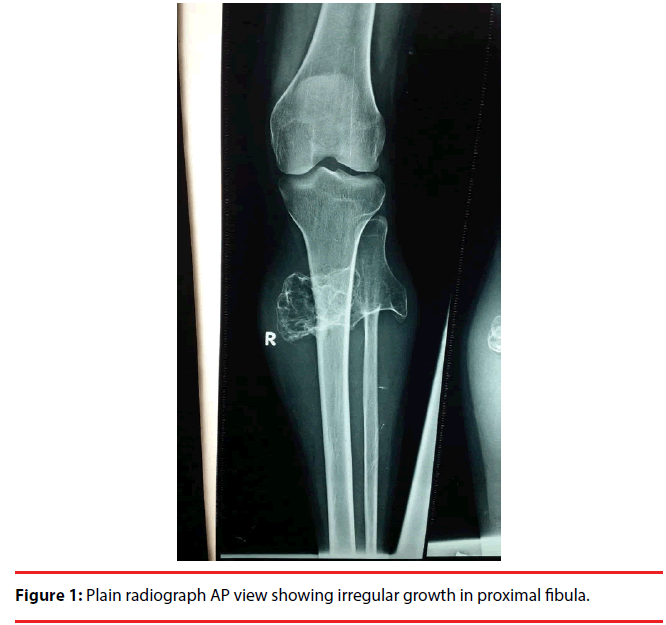
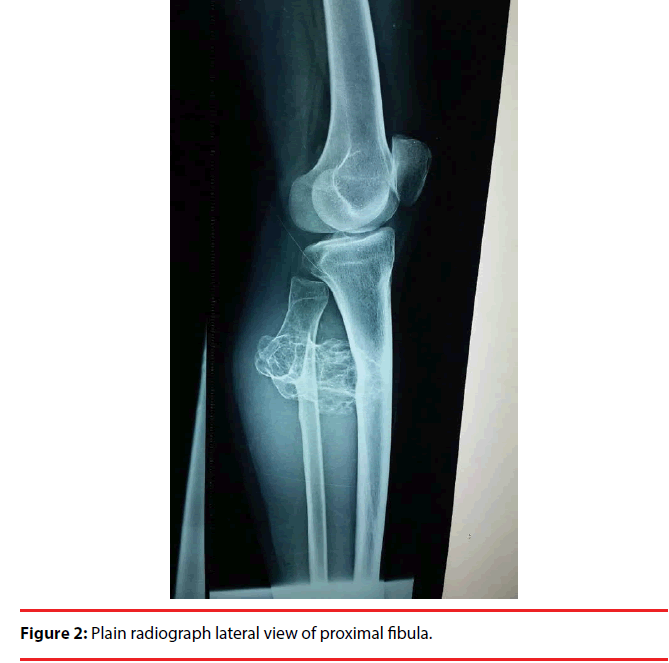
The swelling was fixed to bone, irregular in appearance, hard in consistency, and tender to touch. The swelling was extending to the posterior side of the tibia also and prevent the terminal flexion at the knee joint. There was no distal neurovascular deficit and nerve conduction study showed normal parameters for common peroneal nerve. Plain radiograph showed a large irregular mass arising from the proximal fibula and the major part of the tumour mass had grown medially and posteriorly towards the tibia (Figure 1). Computed tomography showed a large growth arising from the proximal fibula with scalloping of the proximal tibia due to erosion on the posterior surface adjacent to the tumour mass (Figures 2 and 3).
Surgical Procedure
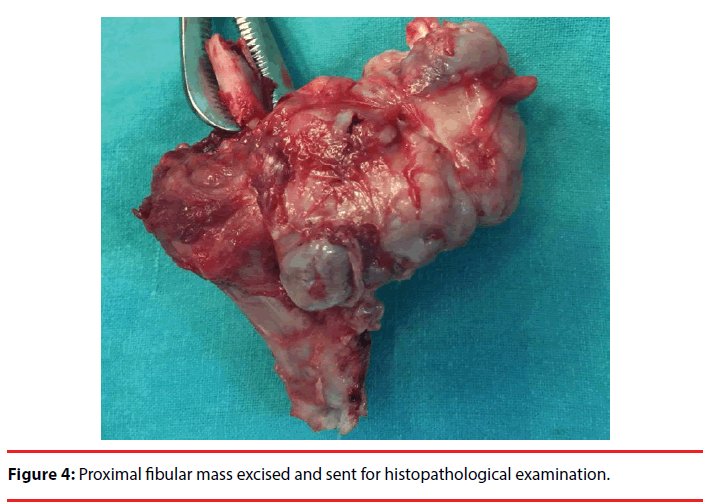
The patient was given combined spinal and epidural block. The tourniquet was applied with patient in supine position. A linear incision of about 5 cm was given along the biceps femoris tendon and then the incision was extended posterior to fibular head and then extended along the fibular shaft (Figure 4). Superficial dissection was done and common peroneal nerve was explored and isolated. Along with it deep peroneal nerve branch were also explored through the fibromuscular tunnel. After this dissection was proceeded distally at the level of planned fibular osteotomy and tumor excision was performed along with removal of fibular head.
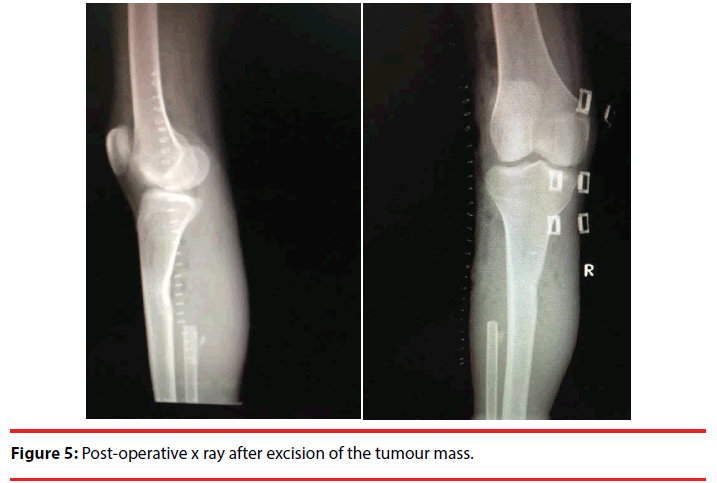
The excised tumour mass was sent for histopathology and it confirmed the diagnosis of osteochondroma and showed no evidence of malignant transformation. The recovery of the patient was uneventful with no distal neurovascular deficit and no complaint of knee laxity on walking. The patient was subsequently followed up which include any wound complication, nerve defect, pain, any abnormal growth and showed no evidence of recurrence of any mass or pain or any neurological deficit after 6 months and 1 year of follow up.
Discussion
Osteochondromas or osteocartilaginous exostoses are the most common benign tumours of the bone [2]. These are benign lesion derived from aberrant cartilage and may take the form of solitary osteochondroma or multiple hereditary exostoses [5].
Solitary osteochondroma usually present as non-tender, slow growing masses. They produce symptom by mass effect over the adjacent structures like bone, nerve, vessels and muscles [6]. Fibula is not a common location for primary bone tumours and the incidence of primary bone tumours in the fibula is 2.5% [3]. Solitary osteochondroma are usually located at the ends of the long bones and present as nontender painless masses [7]. They may continue to grow till the skeletal maturity. Once the physis is fused there growth ceases. Growth in osteochondroma after physeal fusion should arouse the suspicion of malignant changes and should be investigated [8]. These lesion have been reported to spontaneously regress or even resolute during childhood and puberty. The osteocartilaginous growth may be sessile or pedunculated and in 90% of the cases they arise as a solitary lesion. The tumour is mainly composed of bone but the end is usually covered by a cartilaginous cap, which is composed of hyaline cartilage. Osteochondromas commonly present as masses or bony lumps; however, due to their closed vicinity to neuro-vascular bundle can cause compressive neuropathy of peroneal nerve [1] or vascular compression syndrome [2] or a skeletal deformity or pseudoaneurysm of popliteal vessels [4]. A malignant transformation to a chondrosarcoma [approximately 1% for solitary and 20% for patients with multiple lesions] is rare and it should be suspected if tumor is suddenly increasing in size and if there is increase in pain and other symptoms. The diagnoses of osteochondromas are always confirmed by doing radio graphical studies of the affected areas. CT scan and MRI are used to see the bony outline neurovascular status and soft tissue lesions, angiography and colour Doppler may be used to diagnose vascular lesions. Nerve conduction studies are done in the preoperative and post-operative period for assessment of neural function. Bone scans may be helpful in making the diagnosis but they cannot differentiate between benign active osteochondroma and chondrosarcoma because both of them show increased radiotracer uptake. The management is usually surgical with enblock excision of the tumour mass (Figure 5).
In our case the main concern was increase in size of swelling which was causing intense pain and difficulty in movement of knee which was affecting day to day activity of patient. Another concern was of malignant potential of the swelling and its involvement with the surrounding structure such as nerve and vessels. Before excision a CT and colour Doppler was done to rule out any associated vascular lesion. Recurrence after the excision is a rare entity but has been observed and may be attributed to incomplete removal of lesions contiguous with the physis or incomplete removal of cartilaginous cap.
References
- Dahlin DC. Bone tumors, general aspects and data on 6221 cases. Springfield, Charles C. Thomas; 11-12(1978).
- Unni K. Dahlin’s bone tumors: General aspects and data on 11,087 Cases. ed 5. Philadelphia: Lippincot-Raven Publishers(1996).
- Holzapfel BM,Seppel G, Wagner R, et al.Popliteal entrapment syndrome caused by fibular osteochondroma. Ann. Vas.Surg25(7), 982.e5-e10 (2011).
- Malawer MM. Surgical management of aggressive and malignant tumors of proximal fibula. Clin.Orthop.Relat. Res. 1984 (186), 172-181.
- Cardelia JM, Dormans JP, Drummond DS, et al.Proximal fibular osteochondroma with associated peroneal nerve palsy: a review of six cases. J. Pediatr. Orthop15 (5), 574-577(1995).
- Andrikopoulos V, Skourtis G, Papacharalambous G, et al.Arterial compromise caused by lower limb osteochondroma. Vasc.Endovascular.Surg37 (3),185-190 (2003).
- Guy NJ, Shetty AA, Gibb PA. Popliteal artery entrapment syndrome: an unusual presentation of fibular osteochondroma.The.Knee11 (16), 497-499(2004).
- Mnif H, Koubaa M, Zrig M, et al.Peroneal nerve palsy resulting from fibular head osteochondroma. Orthopedics 32(7), 528 (2009).