Effectiveness of Precise Tinnitus Matching and IoTBased Personalized Multimodal Management in the Tinnitus Patients in India
- Corresponding Author:
- Maryam Shojaei Baghini
Department of Electrical Engineering,
Indian Institute of Technology Bombay,
Mumbai,
India,
Tel: 9819869172;
E-mail: mshojaei@ee.iitb.ac.in
Received: 12-Oct-2024, Manuscript No. IJOCS-24-145215; Editor Assigned: 14-Oct-2024, PreQC No. IJOCS-24-145215 (PQ); Reviewed: 28-Oct-2024, QC No. IJOCS-24-145215 (Q); Revised: 14-Dec-2024, Manuscript NO. IJOCS-24-145215 (R); Published: 2211-Dec-2024, DOI: 10.37532/1753-0431.2024.18(3).320
Abstract
Background: Tinnitus is ringing in the ear or head and is a highly prevalent condition affects more than 740 million adults globally and is considered to be a major problem faced by more than 120 million people. The prevalence of tinnitus is about 10% to 15%. The diversified symptoms and customized management requirements further complicate the tinnitus diagnosis and its management. Precise Tinnitus Matching (MyTMD) and IoT based customised management software (TMe-solution) have been demonstrated to be effective in tinnitus management.
Methodology: The study was a single-centre open study, patients aged 18 to 65 years Idiopathic moderate to severe tinnitus or patients with Meniere’s disease with predominant tinnitus symptoms were enrolled. All the patients were asked to revisit the clinical trial centre for efficacy and safety assessment at day 30 and day 60. The primary assessment parameter was the change in the Tinnitus Functional Index (TFI) score at the end of treatment (Day 60) as compared to the baseline. The secondary assessment parameters included changes in the Tinnitus Handicap Inventory (THI) (pretreatment and post-treatment) and changes in Numerical Rating Scale scores (NRS) of loudness, duration, and annoyance at the end of the study.
Results: 11 patients were enrolled in the study. The mean age of the patients was 47.45 years. Female predominance was observed in the patients enrolled in the study (7 women versus 4 men). There was a 58.91% reduction in TFI scores at end of 60 days as compared to the baseline. In the NRS scores there was a trend of progressive reduction of scores of symptoms of ear fullness (24.09% reduction), tinnitus (38.15% reduction), degree of annoyance (60.65% reduction) and duration (53.16% reduction). There was a 61.11% reduction in tinnitus severity score at the end of 60 days.
Conclusion: Management of tinnitus continues to pose a challenge to clinicians. Patients are dissatisfied with the current treatment options. The new tinnitus matching device is a unique non-invasive device offers precise tinnitus matching. The Tinnitus Management software (Tme-solution) allows the patient to be treated with the customized tinnitus masker, Tinnitus Retraining Therapy (TRT), attention diversion technique, CBT using one comprehensive IOT-based platform.
Keywords
Tinnitus; Precise tinnitus matching; Multimodal management
Introduction
Tinnitus is the perception of sound in the absence of any external stimulus. Tinnitus is a phantom sound percept, but phantom percepts are not always associated with pathology [1]. Tinnitus affects more than 740 million adults globally and is considered to be a major problem faced by more than 120 million people [2]. The prevalence of tinnitus is about 10% to 15% [3].
The etiology of primary tinnitus is often unknown. In the secondary tinnitus sound is generated by a source near the ear or referred to the ear, which accounts for less than 1% of tinnitus cases. Examples of the risk factors for tinnitus include increasing age, body mass index of beyond ~30 kg/m2, smoking (former and current), diabetes mellitus, and hypertension [4-7].
Most cases of tinnitus are benign, idiopathic and are strongly associated with sensorineural hearing loss [8]. Tinnitus can be classified qualitatively as non-pulsatile (typically subjective) or pulsatile (often objective) [4,5]. Subjective non-pulsatile tinnitus is the most common and is only heard by the patient. The objective pulsatile tinnitus can sometimes be heard by an observer and is due to an internal bodily vibration or noise. Tinnitus can be unilateral or bilateral. Unilateral tinnitus is caused by cerumen impaction, tympanic membrane perforation, chronic otitis media, otosclerosis, or cholesteatomas, which are also associated with conductive hearing loss. Unilateral tinnitus could also be due to chronic noise exposure, acoustic trauma, semicircular canal dehiscence, or Meniere’s disease, and these patients often have Sensorineural Hearing Loss (SNHL). Some neurological diseases such as multiple sclerosis, cerebellopontine angle tumours, and brainstem infarctions can also cause tinnitus. Bilateral tinnitus is often caused by age related hearing loss, noise exposure, acoustic trauma, otosclerosis and intake of ototoxic medications [9,10].
The severity of tinnitus is heterogeneous, ranging from mildly bothersome to extremely disruptive [1]. Tinnitus has an adverse impact on both physical and psychological well-being. About 1 in 5 patients report that tinnitus interferes with sleep, concentration, or mood. Increasing tinnitus severity is inversely associated with quality of life [11,12]. Often, patients with tinnitus have an increased prevalence of depression and anxiety and cognitive decline [13].
In patients with persistent and bothersome tinnitus, conservative management measures include lifestyle changes to improve sleep, stress reduction, reduce intake of caffeine and alcohol [14,15]. Some patients get relief from hearing aids, which act as a masker by introducing more ambient noise. In the subset of patients in whom basic amplification is not sufficient, specialized tinnitus maskers, including adjustable nature sounds or broadband noise, may offer additional tinnitus relief. Tinnitus retraining therapy, cognitive-behavioral therapy, cochlear implants and transcranial magnetic stimulation are other therapies used to treat tinnitus [16-20]. No effective drug treatments are available and treatment of tinnitus remains unsatisfactory in majority of cases. Surgical management is very rarely used in patients with tinnitus, and its use is restricted to treatable underlying causes such as resection of acoustic neuroma or other brainstem or cerebellopontine angle tumours and lesions, endolymphatic sac shunting for Meniere’s disease, or stapedectomy for otosclerosis [9].
Presently, tinnitus matching is performed with the help of an audiometer by matching the psychoacoustic parameters of perceived tinnitus (such as pitch and loudness). An audiometer can perform tinnitus pitch matching only at seven discrete frequencies as 125, 250, 500, 1000, 2000, 4000 and 8000 Hz and loudness matching in the multiple of 5 dBHL. The tinnitus-matched data (pitch and loudness) obtained from the audiometer is used for sound masking therapy with the help of a tinnitus masker. In many cases the results of masking therapy are non-satisfactory because of the imprecise tinnitus matching with the existing audiometers [21,22].
Tinnitus has to be managed via multimodal approach such as masking therapy, Tinnitus Retraining Therapy (TRT), attention diversion technique, cognitive behaviour therapy, and relaxation techniques, instead of a single solution. The medical guidelines reveal that combined use of therapies are more effective in tinnitus relief. For example, TRT, and sound masking therapy based on measured psychoacoustic parameters in combination with other tactics such as attention diversion, counselling, and relaxation therapy.
A key challenge in the management of tinnitus is the absence of a readily available precise tinnitus matching device which is expected to be small in size, affordable and offers a comprehensive platform and the multi-modal tinnitus management approach.
Mutually coupled tinnitus matching device and tinnitus management software as an assistant set to the ENT doctors and audiologists as well as specific management software for the patients provides the opportunity towards a unique approach for the tinnitus matching and management of tinnitus. In this direction, a new affordable precise tinnitus matching device for the diagnosis of tinnitus has been developed. It also includes an IoT-based multi-modal tinnitus management software for patients. The tinnitus matching device can offer a precise tinnitus sound matching with Pitch resolution of 1 Hz and loudness resolution of 1dB SPL. Moreover, tinnitus management software offers customized multimodal tinnitus management protocols along with diseases progress tracking. The presented device and software in this paper is first benchmarked with respect to the commercially available audiometers and tinnitus management tools. The device and software are used for the study presented in the next section with the results.
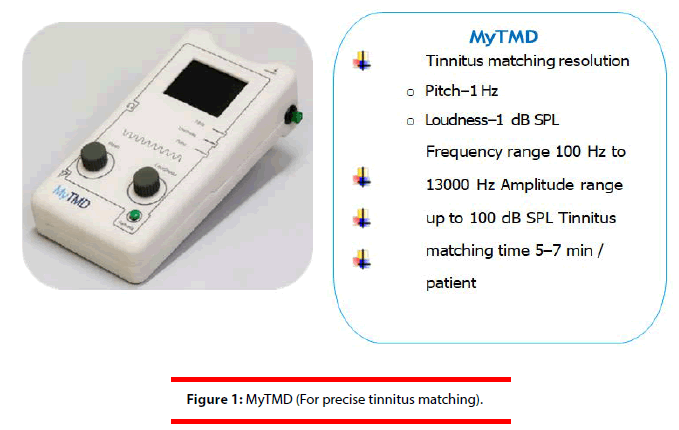
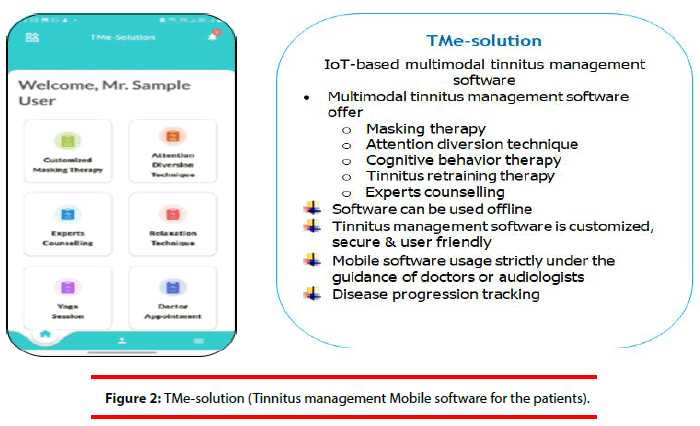
• The novel tinnitus matching device and multi-modal management approach
The Tinnitus Matching Device (MyTMDPrecise tinnitus matching device for doctors and audiologists) and TMe-solution (IoT-based multimodal tinnitus management software for patients) have been designed to be a comprehensive and customized solution for precise tinnitus matching and multi-modal tinnitus management. MyTMD is a new electronic medical device for doctors and audiologists with the pitch resolution of 1 Hz and loudness resolution 1dB SPL. Figures 1 and 2 show the snapshot of MyTMD and The-solution with their features.
The tinnitus matching device is a unique noninvasive device developed to address the challenges posed by the current commercially available audiometers. The tinnitus matching device is intended use to match the tone of tinnitus perceived by patient precisely. The tinnitus management software is a part of the multimodal tinnitus management platform which comprises of various tinnitus management approaches such as customized masking therapy, attention diversion technique, uniform counselling, cognitive behavior therapy by experts, customized tinnitus retraining therapy and relaxation tactics (Figures 1 and 2). All the management tactics are noninvasive and recommended by various national and international societies. Another advantage is that the IOT based platform helps in diseases progress tracking of a tinnitus patients and acts as a useful aid for the doctor for the improved management of tinnitus in their patients.
• Aims
The objectives of this study are to evaluate the efficacy of the precise tinnitus matching device for the diagnosis of tinnitus and to evaluate the safety and efficacy of the tinnitus management software for tinnitus management.
Materials and Methods
The study was a single-centre open study. As per the inclusion criteria, patients aged 18 to 65 years with the one of the following features were enrolled in the study.
• Idiopathic moderate to severe tinnitus
or patients with Meniere’s disease with
predominant tinnitus symptoms.
• Patients who had tinnitus with moderate to
severe sensorineural hearing loss.
11 patients were enrolled in the study. The mean age of the patients was 47.45 years. Female predominance was observed in the patients enrolled in the study (7 women versus 4 men). Three patients had bilateral tinnitus while 8 patients had unilateral tinnitus. One patient had osteoarthritis while one patient had undergone bypass surgery and she had anxiety. Two patients (18%) confirmed they had exposure to noise at work. The mean pulse rate was 77 ± 7.9 BPM. Four patients (36%) had good alertness while 7 patients (63.6%) had normal alertness. Seven patients (63.7%) had a normal appearance, 3 patients (27.2%) had a good appearance and one patient (9%) had a moderate appearance. Mood disturbances were recorded in 5 patients (45.4%). Hearing loss was present in three patients (27.2%). There were no significant otoscopy findings in any patient. 5 patients (45.4%) had unilateral sensorineural hearing loss while one patient had bilateral mild to moderate sensorineural hearing loss and 5 patients (45.4%) had normal findings on audiometry. No adverse effects were reported by any patient.
The patients enrolled in the study had rated the tinnitus as bothersome tinnitus of at least 3 months’ duration, which was not pulsatile, was unilateral or bilateral, and was moderate to severe in intensity (based on the Tinnitus Questionnaire (TQ) score). The exclusion criteria included patients with any anatomic cause of tinnitus, patients with psychiatric disorders, cognitive impairment, active ear disease, pregnant or lactating women, patients with malignancies, patients who had other implantable electronic devices, and patients using commercially available tinnitus maskers. The use of tinnitus management software was explained to the patient. Every patient underwent audiometry before the initiation of the study at baseline and at end of study if deemed necessary [23].
After enrollment in the study, customized therapy was provided after checking the patient on the device. The investigators performed precise tinnitus matching to understand the specific frequency and loudness at which the patient was perceiving tinnitus. All control was given to the investigator. The p atient i nformation w as c onveyed t o t he investigator remotely in real-time through the software. The i nvestigator c ould r emotely a djust the frequency and loudness to match the tinnitus in the patient. Thus i ndividualized t herapy was given to each patient.
All the patients were asked to revisit the clinical trial centre for efficacy and safety assessment at day 30 and day 60. The tinnitus management software was used by the patient two times a day (one use had to be before going to sleep) for a minimum duration of 15-20 minutes and up to a maximum time of use of 90 minutes per day. Attention diversion was for a maximum time period of 60 minutes per day. Patients were evaluated at baseline (day 0), day 30, and day 60. The primary assessment parameter was the change in the Tinnitus Functional Index (TFI) score at the end of treatment (day 60) as compared to the baseline.
The secondary assessment parameters included changes in Tinnitus Symptom Severity (TSS) scores measured with the Tinnitus Handicap Inventory (THI) (pre-treatment and posttreatment) and changes in Numerical Rating Scale scores (NRS) of loudness, duration, and annoyance at the end of the study [24,25]. Safety was assessed by recording adverse effects during the study.
Results
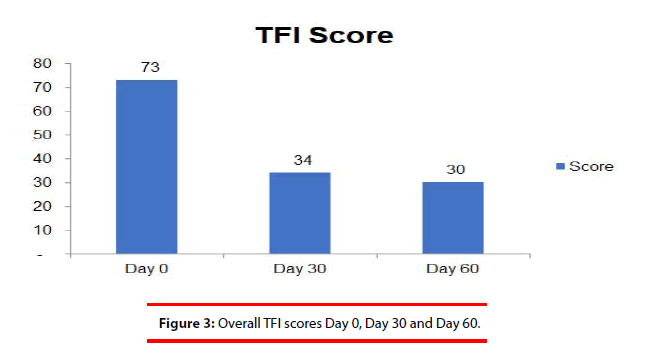
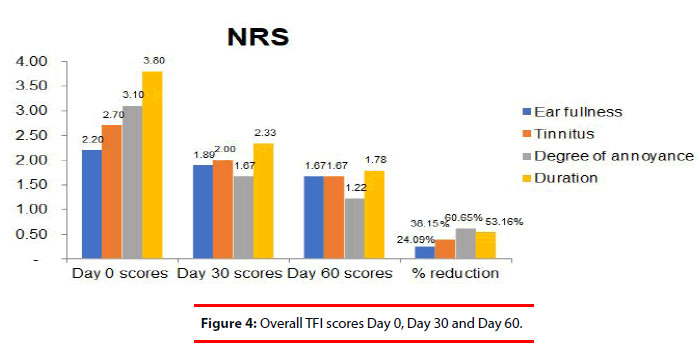
There was a 58.91% reduction in TFI scores at end of 60 days as compared to the baseline (Tables 1 and 2, Figure 3). In the NRS scores there was a trend of progressive reduction of scores of symptoms of ear fullness (24.09% reduction), tinnitus (38.15% reduction), degree of annoyance (60.65% reduction) and duration (53.16% reduction) (Table 3 and Figure 4). There was a 61.11% reduction in tinnitus severity score at the end of 60 days (Table 4 and Figures 5).
| Table 1: TFI scores-subscale analysis (mean) of all enrolled 11 patients. | ||||||||||
| Particular | Day | Overall TFI score | Subscale | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| I: Intrusive (unpleasantness s, intrusiveness, persistence) |
SC: Sense of Control (reduced sense of control) |
C: Cognitive (cognitive interference) |
SL: Sleep (sleep disturbance) |
A: Auditory (auditory difficulties attributed to tinnitus) |
R: Relaxation (interference with relaxation) | Q: Quality of Life (QOL) (quality of life reduced) |
E: Emotional (emotional distress) |
|||
| Mean | Day 0 | 73 | 84 | 85 | 73 | 68 | 59 | 101 | 47 | 71 |
| Std. Dev. | 10 | 8 | 3 | 19 | 20 | 28 | 70 | 29 | 27 | |
| Mean | Day 30 | 34 | 45 | 46 | 36 | 40 | 30 | 32 | 21 | 30 |
| Std. Dev. | 23 | 29 | 31 | 27 | 31 | 22 | 25 | 24 | 22 | |
| Mean | Day 60 | 30 | 36 | 34 | 32 | 30 | 25 | 31 | 28 | 26 |
| Std. Dev. | 21 | 25 | 25 | 27 | 19 | 20 | 23 | 20 | 17 | |
| Reduction Day 0 - | 43 | 48 | 51 | 41 | 38 | 33 | 70 | 19 | 45 | |
| Day 60 | 58.91 | 57.26% | 59.79% | 56.20% | 56.00% | 56.70% | 69.58% | 40.87% | 63.83% | |
| Table 2: Overall TFI scores. | |
| Day | Score |
|---|---|
| Day 0 | 73 ± 10 |
| Day 30 | 34 ± 23 |
| Day 60 | 30 ± 21 |
| % Reduction day 60 vs. day 0 | 58.91% |
| Table 3: NRS scores. | ||||
| Day 0 scores | Day 30 scores | Day 60 scores | % reduction | |
|---|---|---|---|---|
| Ear fullness | 2.2 ± 1.55 | 1.89 ± 1.05 | 1.67 ± 0.87 | 24.09% |
| Tinnitus | 2.7 ± 0.67 | 2 ± 0.71 | 1.67 ± 0.87 | 38.15% |
| Degree of annoyance | 3.1 ± 0.32 | 1.67 ± 0.71 | 1.22 ± 0.67 | 60.65% |
| Duration | 3.8 ± 0.42 | 2.33 ± 0.71 | 1.78 ± 0.67 | 53.16% |
| Table 4: Tinnitus Severity Score (TSS). | ||||||
| Day | Yes | Sometime | No | Overall TSS score | Description | |
|---|---|---|---|---|---|---|
| 4 | 2 | - | ||||
| Mean | Day 0 | 11 | 5 | 4 | 54 | Moderate |
| Std. Dev. | 6 | 5 | 3 | 29 | ||
| Mean | Day 30 | 3 | 8 | 10 | 27 | Mild |
| Std. Dev. | 2 | 6 | 6 | 16 | ||
| Mean | Day 60 | 1 | 8 | 11 | 21 | Mild |
| Std. Dev. | 2 | 5 | 7 | 15 | ||
Discussion
Tinnitus is one of the most common hearing disorders [26]. Tinnitus can be a lifelong disorder and can be associated with annoyance, anxiety, depression, insomnia, hyperacusis, difficulty in concentration. Regardless of the progress made in understanding the etiopathogenesis of tinnitus, management of tinnitus remains a scientific and clinical enigma. No effective drug treatments are available, although much research is underway into mechanisms and possible treatments. The evidence base is strongest for a combination of sound therapy and CBT-based counselling, although clinical trials are constrained by the heterogeneity of patients with tinnitus.
Currently the treatment of tinnitus remains unsatisfactory. No effective drug treatments are available. Tinnitus is managed by using several therapies such as masking therapy, tinnitus retraining therapy, attention diversion technique, cognitive behaviour therapy, and relaxation techniques. Combined use of therapies like Tinnitus Retraining Therapy (TRT), and sound masking therapy based on measured psychoacoustic parameters in combination with other tactics such as attention diversion, counseling, and relaxation therapy are more effective in tinnitus relief.
Patient satisfaction rates are very low, the cost of masking treatment is high and unaffordable to many patients. Moreover, patients have limited access to CBT limited trained audiologists and trained psychologists. The tinnitus maskers generate noise of high frequency which could damage the cochlear cells. The current challenges with tinnitus management include the lack of readily available precise tinnitus matching device, and comprehensive platform for the multi-modal tinnitus management approach, at an affordable cost.
The tinnitus management software overcomes the drawbacks of the current tinnitus maskers. The tinnitus matching software (TMe-solution) provides customized masker that prevents damage to the cochlear cells. It gives the patient access to improved TRT and CBT. The patient learns to ignore tinnitus. Patients in the study reported that they learned to ignore tinnitus and had an improvement in their quality of life.
Another advantage of the tinnitus management software (TMe-solution) is that it allows the patient to be treated with the tinnitus masker, CBT using one comprehensive platform.
The results of this pilot study have indicated a trend towards reduction of symptoms of tinnitus. Patients reported a 60% reduction in degree of annoyance due to tinnitus and 53% reduction in duration of tinnitus. Patients had a 65.75% reduction in TFI scores.
The chief limitation of our study was the small sample size. The results of the current study are promising and a large multi-centric study is warranted to evaluate the efficacy of MyTMD (For precise tinnitus matching) and TMe-solution (Mobile software for patients) in patients with tinnitus.
Conclusion
Management of tinnitus continues to pose a challenge to clinicians. Patients are dissatisfied with the current treatment options. The new tinnitus matching device is a unique non-invasive device offers precise tinnitus matching. The Tinnitus management software (Tme-solution) allows the patient to be treated with the customized tinnitus masker, Tinnitus Retraining Therapy (TRT), attention diversion technique, CBT using one comprehensive IOT based platform.
References
- Henton, A., & Tzounopoulos, T. What’s the buzz? The neuroscience and the treatment of tinnitus. Physiol. Rev. 101, 1609-1632(2021).
[Crossref] [Google Scholar] [PubMed]
- Jarach, C.M., Lugo, A., Scala, M., et al. Global prevalence and incidence of tinnitus: A systematic review and meta-analysis. JAMA Neurol. 79, 888-900(2022).
- Langguth, B. Treatment of tinnitus. Curr Opin Otolaryngol Head Neck Surg. 23, 361-368(2015).
[Crossref] [Google Scholar] [PubMed]
- HJ, H. Epidemiology of tinnitus. Tinnitus: Theory Manag. 16-41(2004).
- Hofmann, E., Behr, R., Neumann-Haefelin, T., et al. Pulsatile tinnitus: Imaging and differential diagnosis. Dtsch Arztebl Int. 110, 451(2013).
[Crossref] [Google Scholar] [PubMed]
- Henry, J.A., Dennis, K.C., & Schechter, M.A. General review of tinnitus: Prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 48, 1204-1235(2005).
[Crossref] [Google Scholar] [PubMed]
- Folmer R.L., Martin, W.H., & Shi, Y. Tinnitus: questions to reveal the cause, answers to provide relief. J Fam Pract. 2004;53(7):532-540.
[Google Scholar] [PubMed]
- Dalrymple, S.N., Lewis, S.H., & Philman, S. Tinnitus: Diagnosis and management. Am Fam Physician. 103, 663-671(2021).
[Google Scholar] [PubMed]
- Cima, R.F., Mazurek, B., Haider, H., et al. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. Hno. 67, 10-42(2019).
[Crossref] [Google Scholar] [PubMed]
- Cianfrone, G., Pentangelo, D., Cianfrone, F., et al. Pharmacological drugs inducing ototoxicity, vestibular symptoms and tinnitus: A reasoned and updated guide. Eur Rev Med Pharmacol Sci. 15,601-636(2011).
[Crossref] [Google Scholar] [PubMed]
- Mohamad,N., Hoare, D.J., & Hall, D.A. The consequences of tinnitus and tinnitus severity on cognition: A review of the behavioural evidence. Hear Res. 332, 199-209(2016).
[Crossref] [Google Scholar] [PubMed]
- Pinto, P.C., Marcelos, C.M., Mezzasalma, M.A., et al. Tinnitus and its association with psychiatric disorders: Systematic review. J Laryngol Otol. 128, 660-664(2014).
[Crossref] [Google Scholar] [PubMed]
- Blazer, D.G., & Tucci, D.L. Hearing loss and psychiatric disorders: A review. Psychol Med. 49, 891-897(2019).
[Crossref] [Google Scholar] [PubMed]
- Wu, V., Cooke, B., Eitutis, S., et al. Approach to tinnitus management. Can Fam Physician. 64, 491-495(2018).
[Google Scholar] [PubMed]
- Langguth, B., Kreuzer, P.M., Kleinjung, T., et al. Tinnitus: Causes and clinical management. The Lancet Neurol. 12, 920-930(2013).
[Crossref] [Google Scholar] [PubMed]
- Sladen, D.P., Frisch, C.D., Carlson, M.L., et al. Cochlear implantation for single‐sided deafness: A multicenter study. The Laryngoscope. 127, 223-228(2017).
[Crossref] [Google Scholar] [PubMed]
- Shekhawat, G.S., Searchfield, G.D., & Stinear, C.M. Role of hearing aids in tinnitus intervention: A scoping review. J Am Acad Audiol. 24, 747-762(2013).
[Crossref] [Google Scholar] [PubMed]
- Hoare, D.J., Adjamian, P., Sereda, M., et al. Recent technological advances in sound-based approaches to tinnitus treatment: A review of efficacy considered against putative physiological mechanisms. Noise Health. 15, 107-116(2013).
[Crossref] [Google Scholar] [PubMed]
- Jastreboff, P.J., Jastreboff, & M.M. Tinnitus Retraining Therapy (TRT) as a method for treatment of tinnitus and hyperacusis patients. J Am Acad Audiol. 11, 162-177(2000).
[Google Scholar] [PubMed]
- Zenner, H.P., Vonthein, R., Zenner, B., et al. Standardized tinnitus-specific individual cognitive-behavioral therapy: A controlled outcome study with 286 tinnitus patients. Hear Res. 298, 117-125(2013).
[Crossref] [Google Scholar] [PubMed]
- Sruthi,N., Venkataramanujam, N.C., Karthikeyan, P., et al. A comparative study of treatment outcomes of music therapy, tinnitus maskers and pharmacotherpy in chronic subjective tinnitus. Indian J Otolaryngol Head Neck Surg. 74, 185-189(2022).
[Crossref] [Google Scholar] [PubMed]
- Fournier, P., Wrzosek, M., Paolino, M., et al. Comparing tinnitus tuning curves and psychoacoustic tuning curves. Trends Hear. 23, 2331216519878539(2019).
[Crossref] [Google Scholar] [PubMed]
- Tunkel, D.E., Bauer, C.A., Sun, G.H., et al. Clinical practice guideline: Tinnitus. Otolaryngol Head Neck Surg. 151, S1-S40(2014).
[Crossref] [Google Scholar] [PubMed]
- Newman, C.W., Jacobson, G.P., & Spitzer, J.B. Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg. 122, 143-148(1996).
[Crossref] [Google Scholar] [PubMed]
- Hallam, R.S. Manual of the tinnitus questionnaire. Polpresa Press. (2009).
- Tang, D., Li, H., & Chen, L. Advances in understanding, diagnosis, and treatment of tinnitus. Hear loss Mec Prev Cure. 109-28(2019).
[Crossref] [Google Scholar] [PubMed]