Determination of Sickle Cell Crisis in Sudanese Children with Sickle Cell Anemia
- Corresponding Author:
- Amged Hussen Abdelrhman
Department of Hematology and Immunohematology
Omdurman Islamic University, Sudan
E-mail: amgedhussen66@gmail. com
Abstract
Abstract
Background: Sickle Cell Anemia (SCA) is a genetic hematological disorder characterized by red blood cells that assume an abnormal rigid, sickle shape. This hereditary disorder contributes the equivalent of 3.4% mortality in children aged under 5worldwide or 6. 4% in Africa.
Methods: Some of red blood cell profile (Hb, PCV, RBCs count and RBCs indices), WBCs count and differential count and platelet count and platelet indices and Hb eletrophoresis were determined by the automated Hematology Analyzer (SysmexBC-3000plus) and reticulocyte count was counted using supravital stain.
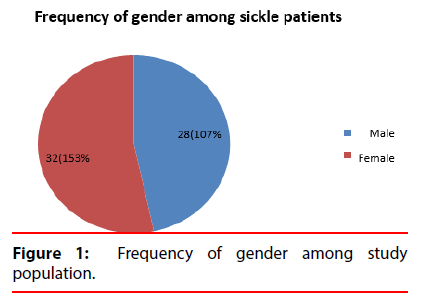
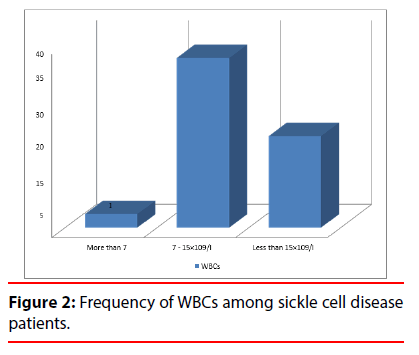
Results: The study was performed on diagnosed 260 children patients with sickle cell disease. Found in this study Frequency of gender among study population in female more than male and insignificant result when Comparison of age, white cells counts, red cells count, hemoglobin, Hematocrit, red cells indices, reticulocyte count and absolute Reticulocyte count among gender of sickle children. Also show insignificant result when Comparison of age, white cells counts, red cells count, hemoglobin, red cells indices, reticulocyte count and absolute Reticulocyte count among age sickle children, however it revealed a significant association with Hematocrit. Significant result show when Comparison of reticulocyte count among hemoglobin group and insignificant absolute Reticulocyte count among hemoglobin group. The Comparison of hemoglobin, reticulocyte count and absolute Reticulocyte count among WBCs. The result show Insignificant. The result were represented significant when Correlation between haemoglobin and reticulocyte count (%).
Conclusion: Insignificant result show when comparison of age, white cells counts, red cells count, hemoglobin, Hematocrit, red cells indices, reticulocyte count and absolute Reticulocyte count among gender of sickle children. The Comparison of white cells counts, red cells count, hemoglobin, red cells indices, reticulocyte count and absolute Reticulocyte count among age group result show insignificant. The Comparison of hemoglobin, reticulocyte count and absolute Reticulocyte count among WBCs. The result show insignificant and also insignificant when correlation between haemoglobin and absolute reticulocyte count. This study concluded to the significant relation between antibiotic use and Monocytes and Basophils. The study Frequency of duration of disease acute, and chronic, and The Frequency of no antibiotic use and antibiotic use. The significant relation between Eosinophils and the symptom and significant relation observed between the Eosinophils and duration of disease. The study showed insignificant correlation between platelet count and platelet indices depending on age, sex and duration of the disease. There was statistically significant Hb F, Hb S in sickle cell individuals.
https://marmarisinvestments.com
https://realestateinmarmaris.com
https://balloonsdocia.com
https://cappadociahotairballoon.org
Keywords
Sickle cell anemia; Crisis; Sickle cell disease; Sudanese children patients
Background
Anemia is a reduction in the hemoglobin concentration of the blood. Although normal values can vary between laboratories, typical values would be less than 13.5 g/dL in adult males and less than 11.5 g/dL in adult females. From the age of 2 years to puberty, less than 11.0 g/dL indicates anemia. As newborn infants have a high hemoglobin level, 14.0 g/dL is taken as the lower limit at birth. Reduction of hemoglobin is usually accompanied by a fall in red cell count and Packed Cell Volume (PCV) [1]. Morphologic classification of anemia: Hypochromic microcytic anemia (low mean cell volume (MCV) low Mean Cell Hemoglobin (MCH)), Normochromic normocytic anemia (normal (MCV), normal (MCH) and Macrocytic anaemia (high MCV). Sickle Cell Anemia (SCA) is a genetic hematological disorder characterized by red blood cells that assume an abnormal rigid, sickle shape [2]. This hereditary disorder contributes the equivalent of 3.4% mortality in children aged under 5 worldwide or 6.4% in Africa. Sickle cell disorders were originally found in the tropics and subtropics but are now common worldwide due to migration of people from the tropical to temperate zone [3,4]. The most common haemoglobin variant in this group is sickle haemoglobin or Hb S. As a result of the replacement of glutamic acid by valine in position 6 of the β chain, Hb S has poor solubility in the deoxygenated state and can polymerize within the red cells. The red cell shows a characteristic shape change because of polymer formation and becomes distorted and rigid, the so-called sickle cell. In addition, intracellular polymers lead to red cell membrane changes, generation of oxidant substances, and abnormal adherence of red cells to vascular endothelium [5].
Sickle cell disease caused by a single point mutation at codon 6 of the globin gene those results in valine, glutamine substitution. Deoxygenated because valine can dock with complementary sites on adjacent globin chains [6]. The abnormal Hb S is soluble and gives no problem when oxygenated. When the oxygen tension decreases, the S hemoglobin polymerizes, forming “tactoids” or “fluid crystals” [7]. The hemoglob+++ in realigns and distorts the red cell into the characteristic sickle shape. The sickling process works in a vicious cycle, once triggered, the cycle builds on itself. The sickle cells in circulation increase the viscosity of the blood, which slows circulation thereby increasing the time of exposure to a hypoxic environment. This promotes further sickling. The formation of rigid sickle cells is likely to plug small circulation, further lowering the PH and oxygen tension and increasing the number of sickled cells [7].
Materials and Methods
▪ Study participants
The study was performed on diagnosed 260 children patients with sickle cell disease in both gender.
▪ Sample preparation and methods
Vein puncture blood sample was collected from the group of study and then putted in EDTA container immediately then was mixed gently. Some of red blood cell profile (Hb, PCV, RBCs count and RBCs indices), WBCs count and differential count and platelete count and platelete indices and Hb eletrophoresis were determined by the automated Hematology Analyzer (SysmexBC-3000plus) and reticulocyte count was counted using supravital stain.
▪ Statistical analysis
Statistical assessment was carried out with Statistical Package for Social Sciences (SPSS) version 17.0 for windows statistical software.
Results
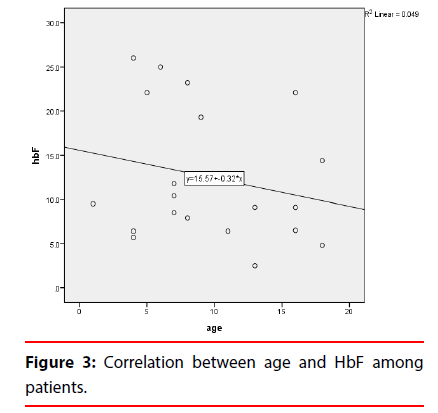
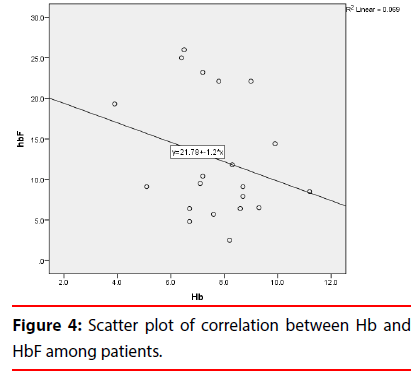
The study showed that among children with sickle cell anemia in Khartoum State, all RBCs indices were low with a marked increase in reticulocyte count (Table 1). This study also showed that the frequency of hemoglobin among the different age groups is less than 7 g/dl in 54 subjects of the age group of <8 years old and more than 7 g/dl in 139 subjects in the same age group. Less than 7 g/dl was found in 114 subjects of the age group of >8 years old and more Than 7 g/dl in 119 subjects in the same age group (Figure 1). The study also revealed that the frequency of WBCs among sickle cell disease patients, 113 patient WBCs less than 7, 137 patients WBCs from 7-15 and 10 patients WBCs more than 15 (Figure 2). There was insignificant association (P value >0.05) between gender and white cells counts, red cells count, hemoglobin, hematocrit, red cells indices, reticulocyte count and absolute reticulocyte count among sickle patients (Table 2). The association of age with white cells counts, red cells count, hemoglobin, red cells indices, reticulocyte count and absolute Reticulocyte count was found to be insignificant (p-value >0.05), However it revealed a significant association with hematocrit (p-value 0.039 ) (Table 3). A significant association (p-value 0.016) was also found between reticulocyte count and hemoglobin level and insignificant absolute reticulocyte count among hemoglobin group (Table 4). The association of hemoglobin, reticulocyte count, absolute reticulocyte count and WBCs was found to be insignificant (p-value>0.05). The result were represented significant (p-value 0.002) when correlation between haemoglobin and reticulocyte count (%). However it revealed an insignificant when correlation between haemoglobin and absolute reticulocyte count. The result show the mean of age among study group (7.4 year), and Mean of TWBCs (7.1 × 109/l), in this study the mean of neutrophils (3 × 109/l), lymphocytes (3.1 × 109/l), monocytes (0.5 × 109/l) (0.5), eosinophils (0.3 × 109/l) and mean of basophils (0.03 × 109/l) (Table 1). In this study the frequency of duration of disease acute (140) Percent (57.1), and chronic (120) (42,9) and the frequency of no Antibiotic use (140) percent (57.1), antibiotic use (120) percent (42.9). The significant relation observed between the eosinophils (p-value 0.023) and duration of disease and the significant relation between antibiotic use and Monocytes (p-value 0.005), and basophils (p-value 0.046) (Table 5), the result according to antibiotic use show insignificant in age (p-value 0.160) and show insignificant in TWBCs (p-value 0.692). The significant relation between eosinophils (p-value 0.003) and the symptoms. The frequency of the platelet count in sickle cell was founded in 126 patients less than 400 (× 109 /l) and more than 400 (× 109 /l) in the remaining 134 patients. The mean of platelet count was insignificant=440.6, MPV (ft)=7.6, P LCR% (11.4) and PDW (ft)=9.2. Comparison of age, platelets count, and platelets indices among gender of sickle patients (Table 6), male=(440.3 ± 194.8); female=(458.3 ± 230.6); p-value=0. 497. MPV (ft) in male=(7.6 ± 0.8); in female (7.6 ± 0. 9); p-value=0.705. P LCR%, in male (11.4 ± 6.2); female (11.5 ± 5.9); p-value=(0.917). PDW (ft) in male (9.4 ± 1.7); female (9.0 ± 1.3); p-value=(0.250). Comparison of platelets count, and platelets indices among age group, the patients less than 8 years; platelet count (× 109 /L)=(464.3 ± 244.6) and patents equal or more than 8 years platelet count (421.1 ± 205.8), p-value=(0.44). MPV (ft) less than 8 years (7.5 ± 0.8), equal or more than 8 years (7.7 ± 0.9), p-value (0.429). P. LCR%, less than 8 years (10.9 ± 5.7) equal or more than 8 years (11.8 ± 6.3), p-value (0.560). PDW (ft) less than 8 years (8.7 ± 1.2) and equal or more than 8 years (9.7 ± 1.6), p-value (0.010). The results of platelet count and in SCD were represent insignificant different with age the p-value (>0.05). Comparison of the platelet indices among the age group were represent insignificant difference with the MPV and P-LCR, but significant with PDW. p-value (0.01). The result of platelet count were represent insignificant value when correlated with age the p-value (0.170). The result of the PMV showed insignificant correlation with age, The p-value (0.225). P-LCR (the p-value (0.273, and significant with PDW (the p-value 0.069). The results were compared according to the objectives of the study as illustrated below (Tables 7 and 8). It show mean and SD of HbF, HbS and HbA2 (12.5 ± 7.5), (84.1 ± 7.3) and (3.0 ± 0.4) respectively, highly significant increase of HbF and HbS according to gender of patients with sickle cell anemia (p-value 0.02, 0.03 respectively). The results show significant positive correlation between the age and HbF (r=0.0.22 p-value 0.02) (Figure 3) and between the HbF and Hb levels (r = 0.2, p-value 0.03) and significant negative correlation between the HbA2 and Hb levels (r=0.04, p-value 0.55) (Figures 4 and 5).
| Parameters | N | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|---|
| Age (years) | 260 | 1 | 14 | 8.5 | 3.6 |
| WBCs (× 109/l) | 260 | 5.2 | 25.4 | 13.9 | 4.9 |
| RBCs (× 1012/l) | 260 | 1.52 | 4.11 | 2.7 | 0.6 |
| Haemoglobin (g/dl) | 260 | 4 | 9.9 | 7.5 | 1.3 |
| PCV (%) | 260 | 14.2 | 29.6 | 23.3 | 3.4 |
| MCV (fl) | 260 | 21.5 | 109.7 | 88.3 | 12.2 |
| MCH (pg) | 260 | 19 | 36.7 | 28.7 | 3.5 |
| MCHC (g/l) | 260 | 26.2 | 35 | 32.1 | 1.8 |
| Reticulocyte count (%) | 260 | 0.3 | 89 | 21.5 | 17.3 |
| Absolute Reticulocyte count (× 109/l) | 260 | 0.7 | 158.3 | 51.9 | 36.9 |
| TWBCs (× 109/l) | 260 | 3.3 | 16.1 | 7.1 | 2.4 |
| Neutrophils (× 109/l) | 260 | 0.8 | 8.9 | 3.6 | 1.7 |
| Lymphocytes (× 109/l) | 260 | 1.4 | 7.2 | 3.1 | 1.2 |
| Monocytes (× 109/l) ) | 260 | 0.1 | 1.6 | 0.5 | 0.3 |
| Eosinophils (× 109/l) | 260 | 0.01 | 1.3 | 0.3 | 0.2 |
| Basophils (× 109/l) | 260 | 0 | 0.2 | 0.03 | 0.02 |
Table 1: Descriptive statistics of study variables.
| Parameters | Gender (Mean ± SD) |
p-value | |
|---|---|---|---|
| Male (n = 28) | Female (n = 32) | ||
| WBCs (× 109/l) | 13.8 ± 5.1 | 15.4 ± 9.7 | 0.477 |
| RBCs (× 1012/l) | 2.5 ± 0.5 | 2.7 ± 0.7 | 0.222 |
| Haemoglobin (g/dl) | 7.5 ± 1.4 | 7.6 ± 1.2 | 0.854 |
| HCT (%) | 22.9 ± 3.7 | 23.7 ± 3.2 | 0.44 |
| MCV (fl) | 90.2 ±7.3 | 86.6 ± 15.1 | 0.243 |
| MCH (pg) | 29.3 ± 2.6 | 28.0 ± 4.1 | 0.191 |
| MCHC (g/l) | 32.5 ± 1.4 | 31.8 ± 2.1 | 0.169 |
| Reticulocyte count (%) | 21.1 ± 11.2 | 21.6 ± 13.2 | 0.932 |
| Absolute Reticulocyte count (× 109/l) | 45.6 ± 36.9 | 57.4 ± 36.4 | 0.222 |
Table 2: Comparison of white cells counts red cells count, hemoglobin, Hematocrit, red cells indices, reticulocyte count and absolute Reticulocyte count among gender of sickle patients.
| Parameters | Age group | p-value | |
|---|---|---|---|
| (Mean ± SD) | |||
| Less than 8 years (n=27) | More than 8years (n = 33) | ||
| WBCs (× 109/l) | 14.8 ± 5.0 | 14.4 ± 9.7 | 0.875 |
| RBCs (× 1012/l) | 2.8 ± 0.6 | 2.6 ± 0.5 | 0.101 |
| Haemoglobin (g/dl) | 7.8 ± 1.1 | 7.2 ± 1.3 | 0.108 |
| HCT (%) | 24.4 ± 3.4 | 22.6 ± 3.3 | 0.039 |
| MCV (fl) | 88.7 ± 9.3 | 87.9 ± 14.0 | 0.813 |
| MCH (pg) | 28.8 ± 3.8 | 28.8 ± 3.2 | 0.829 |
| MCHC (g/l) | 32.1 ± 1.7 | 32.2 ± 1.9 | 0.865 |
| Reticulocyte count (%) | 21.9 ± 10.8 | 21.1 ± 15.1 | 0.869 |
| Absolute Reticulocyte count (× 109/l) | 52.9 ± 35.4 | 51.2 ± 38.5 | 0.858 |
Table 3: Comparison of white cells counts, red cells count, hemoglobin, Hematocrit red cells indices, reticulocyte count and absolute Reticulocyte count among age group.
| Parameters | Hemoglobin (Mean ± SD) | P-value | |
|---|---|---|---|
| Less than 7 g/dl (n=20) | More than 7 g/dl (n=40) | ||
| Reticulocyte count (%) | 28.9 ± 21.3 | 17.7 ± 13.8 | 0.016 |
| Absolute Reticulocyte count (×109/l) | 55.0 ± 34.4 | 50.4 ± 38.4 | 0.654 |
Table 4: Comparison of reticulocyte count and absolute Reticulocyte count with hemoglobin group.
| Parameters | Duration of disease (Mean ± SD) | p-value | |
|---|---|---|---|
| Acute (n=140) | Chronic (n=120) | ||
| Age (years) | 7.2 ± 3.8 | 7.5 ± 3.3 | 0.747 |
| TWBCs (× 109/l) | 7.3 ± 2.8 | 6.7 ± 1.8 | 0.37 |
| Neutrophils (× 109/l) | 3.2 ± 1.9 | 2.7 ± 1.2 | 0.275 |
| Lymphocytes (× 109/l) | 3.1 ± 1.3 | 3.2 ± 1.2 | 0.818 |
| Monocytes (× 109/l) | 0.55 ± 0.25 | 0.51 ± 0.25 | 0.61 |
| Eosinophils (× 109/l) | 0.33 ± 0.26 | 0.22 ± 0.12 | 0.023 |
| Basophils (× 109/l) | 0.03 ± 0.01 | 0.03 ± 0.02 | 0.922 |
Table 5: Comparison of duration of disease and white blood cells.
| Parameters | Age group (Mean ± SD) | p-value | |
|---|---|---|---|
| Less than 8 years (n=127) | Equal or more than 8 years (n=133) | ||
| Platelets Count (× 109/l) | 464.3 ± 244.6 | 421.1 ± 205.8 | 0.441 |
| MPV (fl) | 7.5 ± 0.8 | 7.7 ± 0.9 | 0.429 |
| P-LCR (%) | 10.9 ± 5.7 | 11.8 ± 6.3 | 0.56 |
| PDW (fl) | 8.7 ± 1.2 | 9.7 ± 1.6 | 0.01 |
Table 6: Correlation of age group and platelet count and platelet indices.
| Variable | Mean ± SD Deviation |
|---|---|
| HbF | 12.5 ± 7.5 |
| HbS | 84.1±7.3 |
| HbA2 | 3.0 ± 0.4 |
Table 7: Mean and standard deviation of different hemoglobin types.
| Variable | Male | Female | p-value |
|---|---|---|---|
| Mean ± Std Deviation | Mean ± Std Deviation | ||
| HbF | 14.7 ± 7.2 | 7.7 ± 3.3 | 0.02 |
| HbS | 81.7 ± 7.5 | 89.5 ± 3.2 | 0.03 |
| HbA2 | 3.0 ± 0.53 | 3.1 ± 0.26 | 0.55 |
Table 8: Comparison of different hemoglobin types in both genders.
Discussion
The study showed that among children with sickle cell anemia in Khartoum State, all RBCs indices were low with a marked increase in reticulocyte count. This agrees with result shows, overall mean haemoglobin concentration, packed cell volume, mean cell volume, mean cell haemoglobin, and mean cell haemoglobin concentration in case is low when comparison with control and agrees with [8,9]. Result shows a majority of subjects had demonstrable anemia with increased reticulocytosis. Only increased absolute reticulocyte levels during early infancy were associated with a significant increase in hospitalization during the first three years of life and agrees with [10,11]. Result shows level of WBC was, however significantly higher in patients with HbSS VOC among the SCD, (WBCs are noted in various status of SCD), low in Hb and RBC. There was insignificant association between gender and white cells counts, red cells count, hemoglobin, hematocrit, red cells indices, reticulocyte count and absolute reticulocyte count among sickle patients. This disagrees with [12] result shows mean MCV was higher among HbS subjects but it was only among females and when the result was analyzed irrespective of gender. The association of age with white cells counts, red cells count, hemoglobin, red cells indices, reticulocyte count and absolute reticulocyte count was found to be insignificant, however it revealed a significant association with hematocrit. This disagrees with the result show mean age at diagnosis was significantly lower among males than female [13].
The study showed that the mean of WBCs was not significanted associated with present or absence of infection. This agree with the mean WBCs was not significantly different according to the presence of infection or not, in Regression analyses, the presence of infection was not associated with an increase in total and differential WBCs. Also that white blood cell count is not enough to diagnose severe sickle cell disease this is in an agreement with the study of Derek findings further highlight the poor utility of WBC count by failing to demonstrate an association between WBC count and disease outcomes. Thus, while complete blood counts may help identify complications in those with severe sickle cell diseases, reliance on the WBC count to help guide management decisions should be discouraged. In this study show statistical significant of Eosinophils this result Agree with result of patients with asthma with higher blood Eosinophil counts experienced more asthma attacks than those with lower eosinophil counts. In this study the platelet count and platelet indices showed insignificant deference, and agreed with the results of [14-18]. Also in our study the platelet count and platelet indices showed insignificant deference, and agreed with the results of. However the platelet count and platelet indices showed significant deference, and disagreed with the results of the study. Platelet function was measured on 29 occasions in 16 adult patients in the asymptomatic steady state of sickle-cell anaemia. There was a significant increase in platelet number and micro-aggregate formation, and a lower aggregation threshold with adenosine diphosphate, compared with 23 healthy controls. Similar changes were found, however, in 12 splenectomised patients without sickle-cell diseases. The platelet hyperactivity of the sickle-cell steady state therefore reflects an increased circulating population of young, metabolically active platelet resulting from previous autosplenectomy. The mean of HbS is the larger indicate that most patients have large level of HbS which is the diagnostic hemoglobin for sickle cell anemia. The mean of HbF is increased, while HbA2 is decreased. HbF, HbS and HbA2 show different means and standard deviations in males and females as HbF% in males (14.7 ± 7.2) while in females (7.7 ± 3.3); p-value (0.02); HbS% in males (81.7 ± 7.5) while in females (89.5 ± 3.2); p-value (0.03); HbA2 (%) in males (3.0 ± 0.53) while in females (3.1 ± 0.26); p-value (0.55). This study similar to study which done by Khair FM (Khartoum University) at 2002 in Sudan among sickle cell anemic patient.
Males recorded a higher mean level than females that similar to study. Also, our study agreement with another study of the same fetal hemoglobin is the major genetic modulator of the hematologic and clinical features of sickle cell disease.
Conclusion
A significant association was also found between reticulocyte count and hemoglobin level and insignificant absolute Reticulocyte count among hemoglobin group. The association of hemoglobin, reticulocyte count, absolute Reticulocyte count and WBCs was found to be insignificant. The result were represented significant Correlation between haemoglobin and reticulocyte count (%). This study concluded the importance of screening the white blood cells Count and differential count for children with sickle cell disease when the results of this study are consistent with some previous studies, Significant relation between antibiotic use and Monocytes and Basophils. Significant relation between Eosinophils and the symptom and significant Relation observed between the Eosinophils and duration of disease. The study showed insignificant correlation between sickle cell anemia.
The study showed insignificant correlation between platelet count and platelet indices depending on age, sex and duration of the disease. HbF in sickle cell anemia patients was found to be 12.5% (raised). HbS in sickle cell anemia patients was found to be 84.1%. HbA2 in sickle cell anemia patients was found to be 3.0% (normal).
Declarations
▪ Ethical approval and consent to participant
Approval of this study was obtained from hematology department of medical laboratory science (MLS), Alwatania University, and ministry of health issued by the local ethical committee, Khartoum State, Sudan. Written consent was taken from each member of the study.
▪ Consent for publication
Not applicable.
▪ Availability of data and materials
The datasets generated during and or analyzed in this study are not publicly available due to Bahri Hospital center ethical policy in order to protect participant confidentiality.
▪ Competing interest
The authors declare that they have no competing interests.
▪ Funding
No funding was obtained for this study
▪ Author’s contributions
AH and AA contributed in literature search and manuscript writing. AH had the main idea of the study and contributed in manuscript writing, AA contributed to clinic work, AH contributed in statistical analysis. AA supervised the study and critically reviewed the manuscript. All authors read and approved the final draft of the manuscript.
References
- Hoffbrand PAH, Moss JE, Pettit. Erythropoiesis and general aspects of anaemia. Essential Haematology (5th Ed) 2, 16-20 (2006).
- Charlewd R. The full blood count and classification of anaemi haematology. A Pathogenetic Basis 4, 26 (2003).
- Monica C. Function of s blood haematopoiesis, blood cell disorders. Cambridge University Press, New York (2006).
- Huisman TH. The structure and function of normal and abnormal haemoglobins in: Bailliere's Clin Haematol (1993).
- Harmening DM. Clinical hematology and fundamentals of hemostasis. FA Davis Company (2009).
- Hoffbrand AV, Pttit Je, Moss P. Essential hematology, 4th Ed. Blackwell Science (2001).
- Modell B, Darlison M. Global epidemiology of haemoglobin disorders andderived service indicators. Bull World Health Organ 86, 480-487 (2008).
- Elliot V. Studies on haemoglobin e syndromes. Hematology Am Soc Hematol Educ Program 1, 79-83 (2007).
- Wild BJ, Stephens AD. The use of automated HPLC to detect and quantitate hemoglobins. Clin Lab Haematol 19, 171-176 (1997).
- Vander FP, Volmer M, Gijssel WDG. Predictive value of cord blood hematological indices and hemoglobin barts for the detection of heterozygous alpha-thalassemia-2 in an african-caribbean population. Clin Chem 45, 1495-1500 (1999).
- Lewis S, Bain B, Bales I. Investigation of abnormal haemoglobins and thalassaemia 11th Edn. 14, 303 (2011).
- Robert K, Richard B, Hal J. Nelson textbook of pediatrics. Elsevier 1623-1634 (2007).
- Livingstone Fb. Abnormal hemoglobin in human populations. 1st Edi. 1-490 (2009).
- Ingram Vm. Abnormal human haemoglobins: The comparison of normal human and sickle-cell haemoglobins by fingerprinting. Biochem Biophys Acta 28, 539-545 (1958).
- Keren. Clinical evaluation of hemoglobinopathesis. Warde Med Lab J 14, 3 (2002).
- Lewis SM, Bain JB, Bates I. Practical hematology, 10th Ed, Churchill Living Stone, London (2001).
- Powers Dr, Chan L, Shoeder Wa. The influence of fetal hemoglobin on the clinical expressin of sickle cell anaemia. Ann Ny Acad Sci 505, 262-278 (1989).
- Vella F. Sickling in the western sudan. SMJ 3, 16-20 (1964).