Dental origin Cervical lymphadenopathy: A Rare Case Report.
- Corresponding Author:
- Sghaier Jihed
Department of Oral Medicine and Oral Surgery, University Dental Clinic, Monastir, Tunisia
E-mail: sghaier.jihed25@gmail.com
Received: 29-June-2023, Manuscript No. ijocs-23-104287; Editor assigned: 01-July-2023, PreQC No. ijocs-23-104287 (PQ); Reviewed: 10-July- 2023, QC No. ijocs-23-104287 (Q); Revised: 18-April-2023, Manuscript No. ijocs-23-104287 (R); Published: 27-July2023; DOI: 10.37532/1753- 0431.2022.17(7).313
Abstract
Cervical lymphadenopathy, an intricately multifactorial condition, is one of the foremost prevalent presentation’s dental clinics encounters. Consequently, oral surgeons should possess extensive knowledge regarding the etiology of cervical lymphadenopathy. The present article describes a case of a 60-year-old female who reported to the Department of oral medicine and oral surgery at the University Dental Clinic of Monastir- Tunisia with a complaint of painless swelling of 5 days duration on the right side of her neck, specifically in the jugular-carotid region. The oral examination revealed an infected right maxillary third molar, confirmed on the radiograph. Considering the possibility of neck swelling caused by reactive lymphadenitis secondary to an infected molar, removing the third molar on the right side was performed under antibiotic coverage, which was uneventful. The ultrasound examination, as well as the opinion of the otorhinolaryngologist, confirms the inflammatory origin and absence of signs of malignancy. The patient remained free of the presenting symptoms 28 days later. As well as complete regression of the swelling. The article aims to spotlight the oral physician’s crucial position with inside the early identity of neck swellings, which could bring about well-timed care.
Keywords
Cervical lymphadenopathy, Dental clinics, Malignancy
Introduction
Lymphadenopathy is a common clinical finding for patients seeking dental treatment. It might be local, limited, or general [1]. Cervical lymphadenopathy is thought to be caused by malignancies, infections, autoimmune diseases, iatrogenic, and other miscellaneous conditions [2, 3].
More than half of the patients examined on a daily basis are likely to exhibit enlarged lymph nodes in the head and neck area. The etiology of cervical lymphadenoplasia is varied, so treatment differs from patient to patient [4].
Most cervical lymphadenopathy is caused by a benign infectious etiology; nevertheless, doctors should look for a precipitating reason and examine additional nodal sites to rule out generalized lymphadenopathy
Case Presentation
A 60-year-old female reported to the Department of oral medicine and oral surgery at the University Dental Clinic of Monastir-Tunisia with a complaint of painless swelling of 5 days duration on the right side of the neck, specifically in the jugularcarotid region, with an inflammatory aspect. The patient had diabetes and dyslipidemia and was being regularly treated and followed up by her primary care physician. No history of weight loss or difficulty in swallowing or breathing. There were no dysphagia, dysphonia, laryngeal dyspnea, or night sweats. He reported no relevant history, treatment, known allergy, alcohol or nicotine intoxication, or toxin consumption. Family history showed no recent infections.
The patient presented swelling on the upper part of the right side of the neck, measuring approximately 5 cm × 3 cm in size. On palpation, the swelling was mildly tender, firm, nodular, and mobile with smooth intact overlying skin without any signs of inflammation or infection. Examination of the contralateral side was unremarkable.
Patient consent was obtained for taking a photograph and using it for study and publication purposes (Figure 1).
Intraoral examination revealed poor oral hygiene with the presence of local factors and signs of periodontitis. However, most notably, the right maxillary third molar is decayed and necrotic (Figure 2).
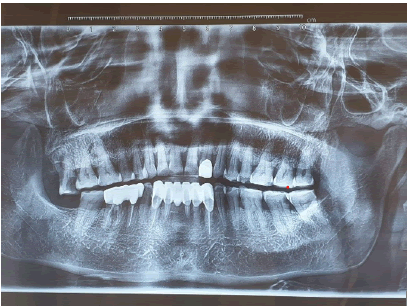
Panoramic radiograph revealed decayed right maxillary third molars, generalized horizontal bone loss, and endodontically treated 31, 32, 33, 43, 45, and 46 with crowns (Figure 3)
Thus, a differential diagnosis of cervical lymphadenopathy due to loco regional infection, toxoplasmosis, and tuberculosis was given by history and clinical examination.
Results of the blood investigations included a raised C - Reactive Protein (CRP) of 8.1 mg/l and raised Erythrocyte Sedimentation Rate (ESR) of 35 mm 1st hour and 73 mm 2nd hour. Tuberculin Skin Test (TST) was negative after exposure to smear-positive tuberculosis.
An ultrasound scan of the neck showed a right-sided, ovoid, well-defined adenopathy of group III, heterogeneous, hypoechoic, with preserved fatty hilum and non-vascularized on color Doppler, measuring 19 mm × 9 mm. It is associated with infiltration and hyperemia of the surrounding soft tissues on color Doppler. Nosigns of necrosis and no visible calcification (Figure 4).
All the investigations were suggestive of benign Reactive adenitis of dental origin. Then, the extraction of the third molar of the right side was performed under antibiotic coverage with a combination of amoxicillin and clavulanic acid (1000 mg twice a day). Swelling completely resolved within the first 10 days of the therapy. But treatment continued as per the protocol. After 20 days of follow-up, she was perfectly all right (Figure 5).
Discussion
Painful neck swelling is a common presenting symptom in adults. Before assessing a neck mass, a comprehensive history of the lesion (location, migration, temporal course, and accompanying symptoms) is collected [5].
While infections are the most common cause of neck masses, neoplasms are the most common cause of persistent neck masses in adults. Malignant neoplasms exceed all other causes of adult neck mass [6].
In general, lymphadenopathy has two mechanisms: hyperplasia and infiltration. The former happens in reaction to immune or infectious stimuli, whereas the latter happens as a result of infiltration by diverse cell types, such as cancer cells, lipid cells, or glycoprotein-laden macrophages.
Lymphadenitis is the pathologic expression of lymph node inflammation. When enlarged lymph nodes are found, a reason can sometimes be discovered by taking a comprehensive medical history, doing a complete physical examination, carefully selecting laboratory testing, and, if required, performing a lymph node biopsy [7].
Lymphadenopathy can be caused by medication responses, infections, immunologic diseases, cancer, and a variety of other conditions with unknown causes [8].
A study conducted between January 1997 and January 2001 investigated the underlying causes of cervical lymphadenopathy in 454 patients who presented with masses in the head and neck region. 61 individuals (13.4%) were diagnosed with cat-scratch disease, 54 (11.9%) exhibited primary lymphadenopathy caused by different infectious agents, and 41 (9.0%) presented with lymphadenopathy associated with primary infections in other organs. In 171 cases (37.7%), the cause of cervical lymph node enlargement remained unidentified [9, 10].
Iqbal et al. showed that 70.45% of cervical lymphadenopathy is due to tuberculosis, 13.63% due to reactive lymphadenitis, 11.36% of cases due to metastases, 4.54% cases due to lymphoma, and 2.27% of cases due to chronic nonspecific lymphadenitis [11].
The diagnosis of Cervical Lymphadenopathy (CLA) etiology should follow a systematic approach, commencing with a comprehensive assessment of the patient’s medical history, thorough physical examination, and, if deemed necessary, further investigative procedures [12].
Complete history taking and physical examination are mandatory for diagnosis; laboratory tests, imaging diagnostic methods, and tissue samplings are the next steps [13]. The importance of patient history varies significantly. It can either lead directly to the reason or propose an explanation, or it might be no diagnostic [14].
The initial goal in determining CLA type is to identify whether it is localized or generalized. The size, consistency, and mobility of the LNs should also be evaluated since they may indicate a malignant character [12].
In cases of localized cervical lymphadenopathy, a thorough evaluation of the draining sites corresponding to the affected levels should be conducted to identify potential sources of infection or malignant disease. If the patient's history and physical examination successfully identify an infection source, further testing may not be required, and treatment can be initiated. However, monitoring for an appropriate response is essential and follow-up care should be ensured [13].
The following factors should be considered during history taking:
• Age: The probability of malignant nature is higher in older age populations.
• Symptoms of infection: Fever, dental pain, ulcers, or discharge.
• Localized symptoms of malignancy: Hoarseness of voice, dysphagia, stridor, ulcers, and pain should be sought.
• Generalized symptoms of malignancy: Weight Loss • Symptoms of the collagen disease: Arthralgia or myalgia.
• Medical history: Allergies to certain drugs are common causes of lymphadenopathy (e.g., phenytoin).
• Occupational and epidemiological exposures: History of high-risk behavior, recent traveling to high-risk regions, or exposure to pets or specific occupational hazards can all suggest a specific underlying etiology
Physical examination is another component of the patient's clinical evaluation.
A complete physical examination involves a thorough inspection of the skin, neck, ears, eyes, nose, and throat. Examine the oral mucosa, tongue, periodontium, and teeth as well [15].
Size is an essential criterion for lymphadenopathy; Lymph nodes bigger than 1 cm in adults or children are not considered normal. Notably, in adults, palpable nodes smaller than 1 cm in the groin are typically regarded as normal [15].
Furthermore, a fixed, immobile node is a classic indicator of malignancy. Tenderness or inflammation above the lymph node indicates an inflammatory condition [16].
Location of enlarged lymph nodes may lead to a source of infection .
Submandibular and submental lymphadenop - athy is most often caused by oral or dental in - fections; cat-scratch disease and non-Hodgkin’s lymphoma.
Pre-auricular and auricular nodes are often enlarged in the presence of ocular disease, rubella, or cat-scratch disease [16].
When supraclavicular nodes are enlarged, there is a strong suspicion of malignant disease, particularly lymphoma or metastatic disease [16]. When general lymphadenopathy is evident, more diagnostic assessment is required, which may involve a biopsy and laboratory testing.
Ordering a Complete Blood Count (CBC) with differential might be beneficial for a practitioner in detecting cases caused by infectious mononucleosis, leukemia, or lymphoma. Neutrophil leukocytosis is often seen in severe infections [17,18].
IgM toxoplasma antibody is the diagnostic serologic test for the acute phase infection of toxoplasmosis [19]. Lymphocytosis can be seen in leukemia, autoimmune disorders, EpsteinBarr virus, cytomegalovirus, and Tuberculosis [20].
Full blood count with hemogram, ESR, CRP, and LDH are helpful in diagnosing malignancies and autoimmune processes [21]. Ultrasonography (US) plays a crucial role in assessing the consistency of enlarged lymph nodes. It serves as a primary diagnostic tool when the clinical examination alone is insufficient to determine the nature of the lymph nodes. The primary objective of the ultrasonographic examination is to differentiate between reactive, tuberculous, lymphomatous, and metastatic etiologies of the lymph nodes [13].
Other means of adjunctive evaluation may include lymph node aspiration, Fine-Needle Aspiration Biopsy (FNAB), or excisional biopsy [17].
Infections arising in the teeth and oral tissues can migrate to the head and neck region via the lymphatic system. This is made possible by the lymphatics, which connect a number of nodes and allow germs to circulate in the lymph fluid [22].
The route of dental infection traveling through the nodes varies according to the teeth involved [23]. The primary nodes for the maxillary third molars and the associated tissues, as in our case, are the superior deep cervical nodes. The superior deep cervical nodes empty into either the inferior deep cervical nodes or directly into the jugular trunk and then into the vascular system [23].
Oral infection accompanied by evidence of systemic spread like lymphadenopathy requires antibiotic therapy. The type of antibiotic chosen and its dosing regimen is dependent upon the severity of the infection and the predominant type of causative bacteria [24].
Clindamycin or a combination of amoxicillin and clavulanic acid should be used to treat patients who have cervical lymphadenopathy and periodontal or dental disease since these antibiotics offer coverage for anaerobic oral bacteria [25].
Depending on the clinical response of the present treatment, antimicrobial therapy may need to be adjusted after a causal agent is discovered.
Failure of regression of lymphadenopathy after 4 to 6 weeks might be an indication for a diagnostic biopsy [26].
Conclusion
This case study emphasizes the significance of appropriate examination, particularly of lymph nodes, and the use of many diagnostic modalities for accurate disease diagnosis. As oral healthcare professionals, we are responsible for safeguarding our patients’ oral and overall health. Therefore, we must identify early signs of systemic diseases and deliver appropriate patient care.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy
Acknowledgements
Authors are grateful to the patients for their collaborations.
Authors’ Contributions
All authors have read and agreed to the final version of this manuscript and have equally contributed to its content and to the management of the cases.
Ethical Approval
As per international standard or university standard written ethical approval has been collected and preserved by the authors.
References
- Ochicha O, Edino ST, Mohammed AZ, et al. Pathology of peripheral lymph node biopsies in Kano, Northern Nigeria. Ann. Afr. Med. 6, 104 (2007).
- Upadhyay, Nitin, Anand Chaudhary, et al. Cervical lymphadenopathy. J Dental Sci 30-33(2012).
- Aw, Bazemore. Smucker DR. Lymphadenopathy and malignancy. Am Fam Physician 66, 2103-10(2002).
- Ramadas AA, Jose R, Varma B, et al. Cervical lymphadenopathy: Unwinding the hidden truth. Dent. Res. J. 14, 73 (2017).
- Ramadas, Athira Aruna . Cervical lymphadenopathy: Unwinding the hidden truth. Dent. Res. J. 14, 73 (2017).
- Olsen, Kerry D. Evaluation of masses in the neck. Primary Care: Clin. Off. Pract. 17, 415-435 (1990): 415-435.
- Linet, Otto I, Carl Metzler. Practical ENT: incidence of palpable cervical nodes in adults. Postgrad. med. 62.4 (1977): 210-213.
- Pangalis GA, Vassilakopoulos TP, Boussiotis VA. Clinical approach to lymphadenopathy. Seminars in oncology. 20(1993).
- Ridder, Gerd Jürgen, Grunow R et al. Role of cat-scratch disease in lymphadenopathy in the head and neck. Clinical infectious diseases 35, 643-649(2002).
- Ridder, Gerd Jurgen . Role of cat-scratch disease in lymphadenopathy in the head and neck. Postgrad. med. 35, 643-649 (2002)
- Channa, Muhammad Ali . Frequency of tuberculosis in cervical lymphadenopathy: our experience. (2010).
- Ferrer, Robert. Lymphadenopathy: differential diagnosis and evaluation. Am. fam. physician 58, 1313-1320(1998).
- Sakr, Mahmoud. Cervical: Lymphadenopathy. Head and Neck and Endocrine Surgery: From Clinical Presentation to Treatment Success 163-190(2016).
- Lee, YEUâÂÂTSU N., Roger Terry, and Robert J. Lukes. Lymph node biopsy for diagnosis: a statistical study. J. surg. oncol. 14, 53-60(1980).
[Google Scholar] [Crossref]
- Parisi E, Glick M. Cervical lymphadenopathy in the dental patient: a review of clinical approach. Quintessence Int. J 36,423-36(2005).
- Leung, Alexander KC, and H. Dele Davies. Cervical lymphadenitis: etiology, diagnosis, and management. Curr. infect. dis. rep. 11, 183-189(2009).
- Ying M, Ahuja AT, Evans R, et al. Cervical lymphadenopathy: sonographic differentiation between tuberculous nodes and nodal metastases from non–head and neck carcinomas. J. clin. ultrasound 26, 383-389(1998).
- Mohseni Sh, Shojaiefard A, Khorgami Z,et al. Peripheral lymphadenopathy: approach and diagnostic tools ,Iran. j. med. sci. 39, 158(2014).
- Ferrer R. Lymphadenopathy: differential diagnosis and evaluation. Am Fam Physician.58, 1313-20(1998). PubMed PMID: 9803196.
- Haque Au, Aan Nu. Leukemoid Reaction: Unusual Causes. Int. J. Pathol.8,39-40(2010).
- Richner, Silvia. Peripheral lymphadenopathy in immunocompetent adults. Swiss Medical Weekly. 140, 98-104(2010).
- Harness, Neil G. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. JBJS. 86, 1900-1908(2004):.
- Fehrendbach MJ, Herring SW. Illustrated Anatomy of the Head and Neck. Philadelphia. 1996.
- Dar-Odeh, Najla Saeed. Antibiotic prescribing practices by dentists: a review. Ther. clin. risk manag. 6, 301(2010).
- Peters, Timothy R, Kathryn M. Edwards. Cervical lymphadenopathy and adenitis. Pediatr. rev. 21, 399-405(2000).
- Papadopoulos, Evangelic. Cervical lymphadenopathy in childhood epidemiology and management. Pediatr. hematol. oncol. 26, 454-460(2009).