Cold Hands Warm Heart: Does Hand Rubbing Really Make A Difference?
- Corresponding Author:
- Charlotte Katharine Gunner
Department of General Surgery
Sheffield Teaching Hospitals NHS Foundation Trust, United Kingdom
E-mail: charlottegunner@gmail.com
Abstract
Objective: An abdominal examination by a physician with cold hands is perceived to produce patient discomfort. In an attempt to alleviate
this discomfort the clinician’s examining hands are traditionally rubbed together. However, it is unknown whether these brief ‘hand rub’
results in a clinically relevant change in hand temperature.
Design: Non-randomized trial
Setting: Multicenter study
Participants: 71 members of clinical staff
Main Outcome Measure: Palmar temperature change after vigorous hand rubbing for 2 and 10 seconds.
Results: The baseline median (IQR) palm temperature was 30.9 ± 1.4°C. Two seconds of hand rubbing increased the palmar temperature by
0.2°C to 31.1 ± 1.2°C (p=0.11; Mann-Whitney U test). Ten seconds of hand rubbing raised the palmar temperature by 0.4°C to 31.3 ± 1.3°C
(p=0.02; Mann-Whitney U test).
Conclusion: A brief but vigorous hand rub immediately prior to examination of a patient’s abdomen does not produce a clinically meaningful
rise in hand temperature.
Keywords
Clinical examination; Hands; Rubbing; Temperature; Comfort
Introduction
The old adage that cold hands often conceal a warm heart was dispelled by Williams and Bargh, who demonstrated that physical warmth, promotes interpersonal warmth [1]. The warmth of personality aside, cold hands are a common finding amongst doctors carrying out physical (especially abdominal) examinations, with the phrase ‘I’m sorry my hands are a bit cold’ often followed by a sharp intake of breath from the patient upon skin contact. In an attempt to alleviate this perceived discomfort it is common for a brief ‘palm-to-palm’ hand rub to be performed by the clinician in an effort to warm the hands immediately prior to the examination. As the generation and maintenance of palmar warmth following a cursory hand rub are unlikely to be significant, we, therefore, investigated whether this brief hand rub was able to generate a clinically significant rise in hand temperature.
Methods
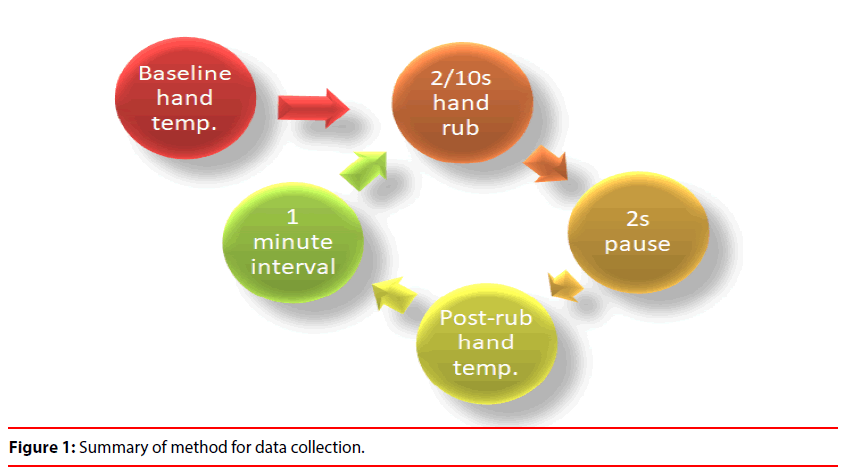
Test subjects (nurses, operating theatre staff, junior doctors and consultants) were recruited at random on multiple days in summer from two separate hospitals. Subjects were instructed to rub their hands together vigorously for 2 seconds. Palmar temperature was then recorded at a distance of 2 cm using a non-contact infrared thermometer (Dodocool GM300; temperature range -50 to 380 degrees Centigrade). All measurements were taken 2 seconds after completion of the hand rub and were repeated in triplicate with an interval time of 1 minute between each recording. The entire process was then repeated using a 10 second, rather than a 2 second, hand-rub. All measurements were taken in degrees Centigrade. The study design is summarised in Figure 1.
A power calculation demonstrated that, with an α of 0.05, a sample size of 50 would be required to detect a difference of 0.4°C with a power of 80%. Temperature differences between groups were analyzed using the Mann-Whitney U test.
Results
71 subjects (39 female, 32 male; median [range] age 24 [20-55] years) were recruited. Initial pilot data demonstrated less variability when recording palmar temperature than finger temperature. Therefore throughout the main study, all measurements were taken from the central palmar area of the right hand at a distance of 2 cm.
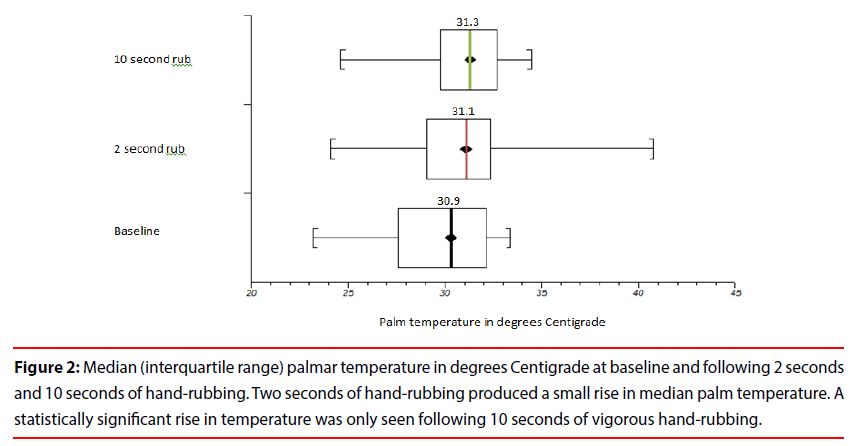
Median (interquartile range) baseline palm temperature was 30.9 (29.5-32.3)°C.
There was no statistical difference between baseline palmar temperature and palmar temperature after 2 seconds of hand rubbing (median [IQR] temperature 31.1 [29.1-32.3]°C; p=0.11). Ten seconds of hand-rubbing produced a small but significant rise in palm temperature (median [IQR] temperature 31.3 [29.8-32.6]°C; p=0.02).
Results are presented graphically in Figure 2.
Figure 2: Median (interquartile range) palmar temperature in degrees Centigrade at baseline and following 2 seconds and 10 seconds of hand-rubbing. Two seconds of hand-rubbing produced a small rise in median palm temperature. A statistically significant rise in temperature was only seen following 10 seconds of vigorous hand-rubbing.
Discussion
Although a warm hand prior to abdominal examination is advocated in standard clinical examination textbooks [2], it has never previously been investigated whether hand rubbing is an appropriate means to achieve this. We demonstrate, for the first time, that the commonly observed brief hand rub is an ineffective means of producing a rise in palm temperature and hence believe the process has no scientific merit.
Significant efforts were made in the study design to reflect current clinical practice. Covert pilot observational data demonstrated that the duration of hand-rubbing rarely exceeded 2 seconds, and this period was therefore chosen for the initial data collection. To simulate the time taken in clinical practice between hand rubbing and patient contact a 2-second delay was instituted for all recordings. Furthermore, the performance of the study during the British Summer (traditionally a time of persistent cold rain) ensured the coolness of study subjects’ hands prior to participation in the study.
Hand rubbing vigorously for 10 seconds was noted to produce a minor, yet statistically significant, change in palm temperature of 0.4°C. At the age of 40 years, the lowest temperature change discernible by abdominal skin is 0.4°C [3]. However, the sensitivity of abdominal skin to recognize temperature changes deteriorates markedly with age 3, and therefore even 10 seconds of hand rubbing does not create a clinically significant difference in hand temperature when examining patients over the age of 40 years. Moreover, in our experience even the most zealous of hand-rubbing clinicians are unlikely to utilize a vigorous hand rub of 10 seconds.
We have not explored the psychological aspects of hand rubbing; doctors may be perceived as more empathetic towards their patients and are seen to make an effort to reduce discomfort from cold hands. In a similar manner exhalation onto a stethoscope prior to auscultation is commonly seen, particularly in pediatric practice. However, evidence to support these observations as a proven means of emotional warmth on the part of the healthcare professional is lacking.
Conclusion
The commonly observed practice of a brief hand-rub prior to abdominal examination is an ineffective means of raising hand temperature.
Competing Interests
None
Authorship
CG designed the study, coordinated data collection, and analysis and wrote the article. ML analyzed the data and edited the article. AB and HC collected data and increased the vigor of subject hand-rubbing through enthusiastic encouragement. OS edited the article and submitted it. KC was responsible for the study’s conception. He also contributed to study design, data analysis, and article editing.
References
- Williams LE, Bargh JA. Experiencing physical warmth promotes interpersonal warmth. Science 322(5901), 606-607 (2008).
- Glynn PM, Drake WM, Hutchison RS. Hutchinson’s clinical methods: An integrated approach to clinical practice with student consult online access. Elsevier Health Science (2012).
- Stevens J, Choo KK. Temperature sensitivity of the body surface over the life span. Somatosens Mot Res 15(1), 13-28 (1998).