An uncommon etiology of nausea and vomiting: paraesophageal hernia
- Corresponding Author:
- Tokunbo Ajayi
Department of Internal Medicine, 81 Highland Ave NSMC, Salem, MA, USA
Tel: 206-832- 7770
E-mail: tajayi@mgh.harvard.edu
Abstract
A 62 year old female on omeprazole with a history of hiatal hernia, gastroesophageal reflux disease (GERD), and esophagitis presented with acute onset of nausea and vomiting. She vomited approximately 20 times, quantified as half a cup mixed with dark red blood. Initially, the emesis was all recently ingested meals. The emesis became bloody after 24 hours of vomiting, leading to her presentation in the ER. She continued to feel nauseous with belching in the ER. She denied any abdominal pain, diarrhea, constipation, chest pain, odynophagia or shortness of breath. She had no melena, hematochezia, fevers, chills or weight loss. She denied any NSAID use or recent international travel. She had no family history of gastrointestinal malignancy and no history of tobacco use. Her physical examination and vital signs were unremarkable. Laboratory data was significant for white cell count of 18.78 K/µL, hemoglobin of 15.7 G/DL, hematocrit 46.3% (hemoglobin & hematocrit at baseline), mean corpuscular volume 88FL, platelet count 65 K/µL and INR was 1.0. Her chemistry, liver function test, lipase and amylase were within normal limits. Computed tomography(CT) scan of the chest was done.
https://bluecruiseturkey.co
https://bestbluecruises.com
https://marmarisboatcharter.com
https://bodrumboatcharter.com
https://fethiyeboatcharter.com
https://gocekboatcharter.com
https://ssplusyachting.com
Keywords
Hematochezia, Computed tomography, Melena
Introduction
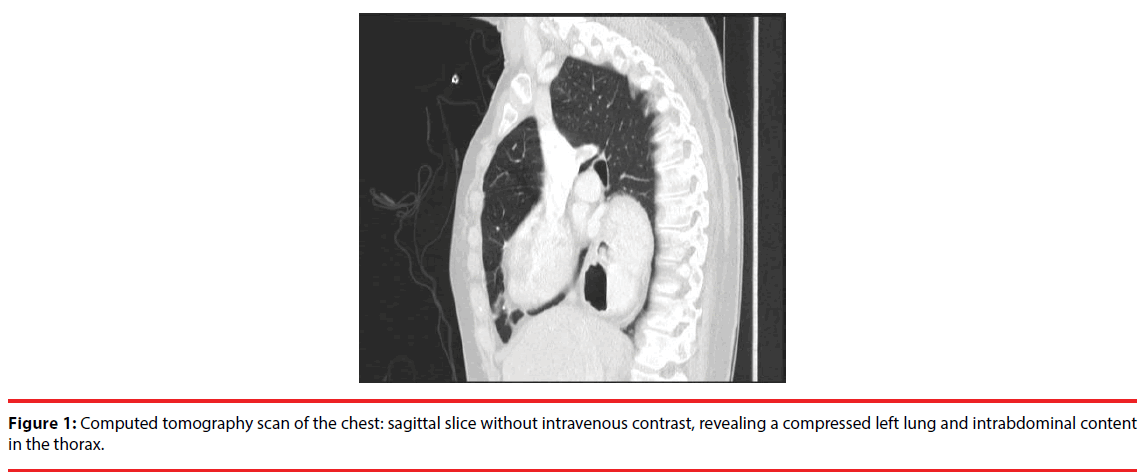
A 62 year old female on omeprazole with a history of hiatal hernia, gastroesophageal reflux disease (GERD), and esophagitis presented with acute onset of nausea and vomiting. She vomited approximately 20 times, quantified as half a cup mixed with dark red blood. Initially, the emesis was all recently ingested meals. The emesis became bloody after 24 hours of vomiting, leading to her presentation in the ER. She continued to feel nauseous with belching in the ER. She denied any abdominal pain, diarrhea, constipation, chest pain, odynophagia or shortness of breath. She had no melena, hematochezia, fevers, chills or weight loss. She denied any NSAID use or recent international travel. She had no family history of gastrointestinal malignancy and no history of tobacco use. Her physical examination and vital signs were unremarkable. Laboratory data was significant for white cell count of 18.78 K/μL, hemoglobin of 15.7 G/DL, hematocrit 46.3% (hemoglobin & hematocrit at baseline), mean corpuscular volume 88FL, platelet count 65 K/μL and INR was 1.0. Her chemistry, liver function test, lipase and amylase were within normal limits. Computed tomography(CT) scan of the chest was done (Figure 1).
What is your diagnosis?
• Oesophageal cancer
• Cardiac tumour with compression on the oesophagus
• Paraesophageal hernia with gastric volvulus
• Lung cancer with compression on the oesophagus
• Mallory Weiss tear
Discussion
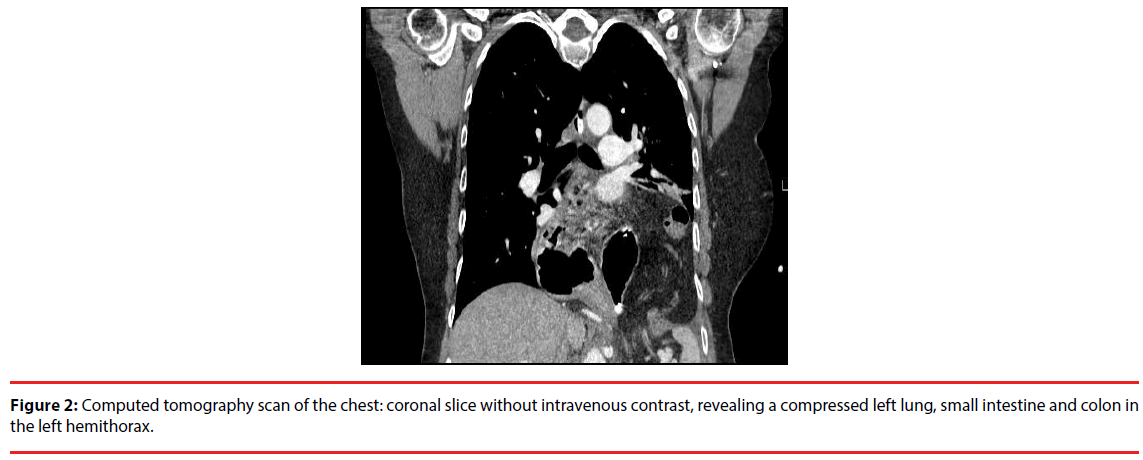
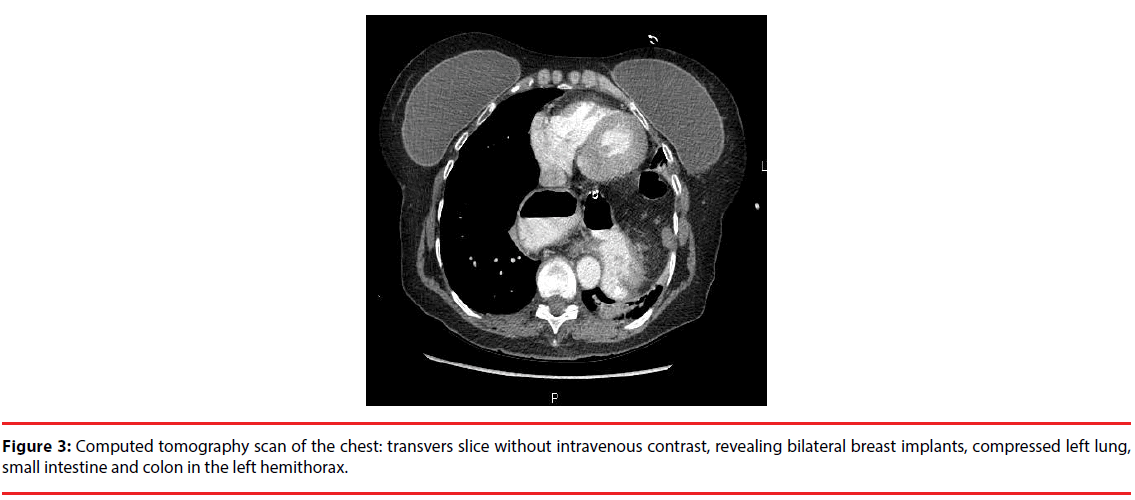
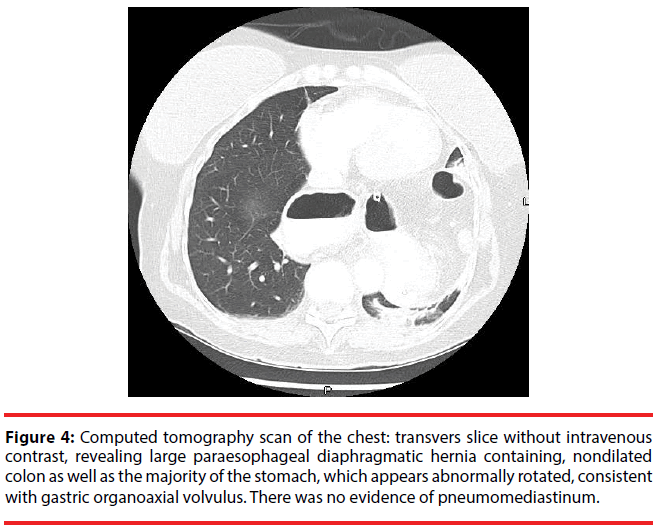
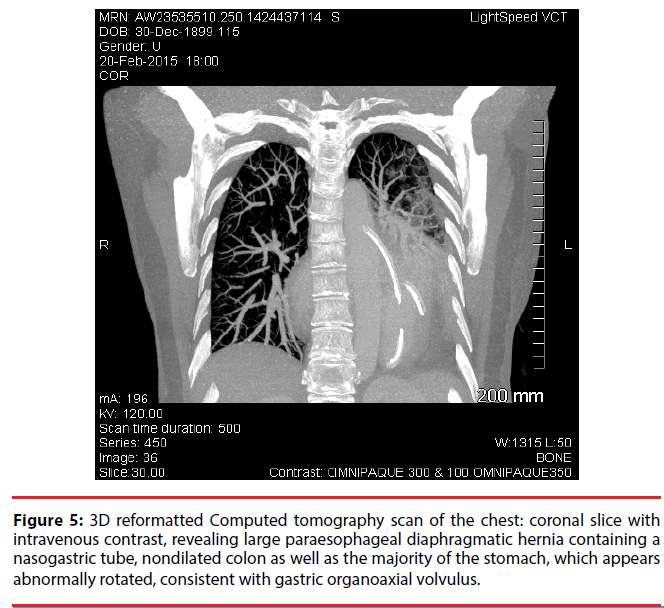
The answer is (c) paraesophageal hernia with gastric volvulus. The diagnosis was made based on the patient’s clinical history, results of the CT and findings on the endoscopic gastroduodunoscopy. Our patient was initially managed as a case of Mallory-Weiss tear versus recurrence of her esophagitis; she was started on IV pantoprazole, ondansteron and IV normal saline. Her EGD showed torsion at the gastroesophageal junction with concern for gastric volvulus versus incarcerated paraesophageal hernia as there was resistance with passage of EGD probe. Chest CT (Figures 2-5) confirmed a large paraesophageal diaphragmatic hernia containing nondilated colon and the majority of the stomach. The stomach appeared abnormally rotated, consistent with gastric organoaxial volvulus. There was no evidence of pneumomediastinum. She underwent laparoscopic repair of incarcerated type IV paraesophageal hiatal hernia with a partial posterior hiatoplasty with mesh placement (11 × 14 cm Ventrio ST hernia patch) and Nissen fundoplication. She was discharged 2 day post op after tolerating full liquid diet.
Figure 4: Computed tomography scan of the chest: transvers slice without intravenous contrast, revealing large paraesophageal diaphragmatic hernia containing, nondilated colon as well as the majority of the stomach, which appears abnormally rotated, consistent with gastric organoaxial volvulus. There was no evidence of pneumomediastinum.
Figure 5: 3D reformatted Computed tomography scan of the chest: coronal slice with intravenous contrast, revealing large paraesophageal diaphragmatic hernia containing a nasogastric tube, nondilated colon as well as the majority of the stomach, which appears abnormally rotated, consistent with gastric organoaxial volvulus.
Hiatal hernias are generally benign; however, a type IV paraesophageal hernia is rare and usually not a benign finding. It includes a peritoneal layer that forms a true hernia sac which distinguishes it from the more common sliding hiatal hernia [1]. It is estimated that greater than 95% of hiatus hernias are type I, with type II to IV hernias accounting for approximately 5% [1-3]. Hiatal hernias are classified into one of four types:
• Type I is a sliding hernia and is characterized by the displacement of the gastroesophageal (GE) junction above the diaphragm. The stomach remains in its usual longitudinal alignment and the fundus remains below the GE junction [2].
• Type II hernias result from a localized defect in the phrenoesophageal membrane where the gastric fundus serves as a lead point of herniation, while the GE junction remains fixed to the preaortic fascia and the median arcuate ligament [2].
• Type III hernias have elements of both types I and II hernias. They are characterized by both the GE junction and the fundus herniating through the hiatus. The fundus lies above the GE junction [2].
• Type IV hiatus hernia is associated with a large defect in the phrenoesophageal membrane and is characterized by the presence of organs other than the stomach in the hernia sac (e.g., colon, spleen, pancreas, or small intestine)[2].
PH are frequently asymptomatic or associated with vague and intermittent symptoms of gastroesophageal reflux [1-5]. Paraesophageal hernia can be complicated by development of gastric volvulus, gastric outlet obstruction, hemorrhage, and, rarely, respiratory compromise in the setting of compression of the left main stem bronchus [1], such complication is an indication for emergent surgery.
Chest x-ray or CT abdomen/pelvis is the imaging modality used in the diagnosis of a PH and is usually performed for reasons other than gastroesophageal reflux. Patients with symptomatic gastroesophageal reflux are typically evaluated by an upper endoscopy and/ or video barium swallow. Prior to surgical repair, all patients diagnosed with a PH should undergo endoscopic evaluation [1-5].
Based on the Society of American Gastrointestinal and Endoscopic Surgeons (SAGE) guidelines treatment is directed towards symptoms of gastroesophageal reflux (GERD) which is one of the common medical consequences of a hiatal/ paraesophageal hernia. Surgical management is indicated when medical management fails to control symptoms of GERD that may be related to the PH, or when complication develops as seen in our patient [2,6,7].
Indications for an elective repair of a paraesophageal hernia include failed medical management of GERD, dysphagia, early satiety, postprandial pain, anemia, and vomiting associated with a PH. The strength of these recommendations is rated strong and quality of the evidence as high by SAGE. Our patient developed gastric volvulus as a complication of PH requiring emergent surgery. The mortality rate of elective laparoscopic paraesophageal hernia repair is estimated at 1.4% [6-8].
Differential Diagnosis
Differntial diagnosis for nausea and vomiting is numerous from local etiology to systemic reason. However when there is concern for obstruction it can be narrowed down into luminal etiology and extraluminal etiology. Our differntial diagnosis is listed in Table 1.
| Condition | Characteristics |
|---|---|
| Mallory Weiss tear | Severe nause, vomiting, retching and hematemsis. Seen in alcoholics,older age and hiatal hernia. Confirmed with an EGD. Acute presntation |
| Paraesophageal hernia | Severe form of hiatal hernia. nause, vomiting, retching and hematemsis. Difficulty to pass the EGD probe.Abdominal content seen in the thorax. Can be acute or chronic. |
| Esophageal cancer | Seen in elderly, smokers. Nausea, vomiting, dysphagia, weight loss. Usually present with acute on chronic symptoms. Lesion seen on EGD |
| External mediastinal compression(mass, cancer, vasculature) | Nausea, vomiting, dysphagia, weight loss. Specific symptoms based on organ compressing the GI tract. Imaging will help with diagnosis. Usually present with acute on chronic symptoms. |
Table 1: Selected Differential Diagnosis of Paraesophageal hernia.
Oesophageal cancer is less likely in our patient because of the acute of the symptoms which started with one day prior to presentation. There was no associated weight loss. The patient had no smoking history which is a significant risk factor for head and neck malignacies. She did have hematemesis which could be an harbinger for malinancy. However, this can be explained by continous retching leading to mucusal injury. Finally the EGD did not show any mass or pre-malignant lesion such as barrett’s esophagus as patient has history of GERD. External compression of the esophagus by mediastinal structure can lead to obstruction causing nausea and vomiting as seen in our patient. Cardiac mass or dilatation of cardiac chambers or aberrant vasculature could cause this compresion. This is less likely in our patient has she did not have any typical cardiac symptoms such as chest pain, shortness of breath, leg swelling or weight loss.There was no mediastinal mass or cardiac vasculature compressing the esophagus on CT. Lung cancer with or without metastasis is another possible differntial; however, without respiratory symptoms, weight loss or CT findings it is less likely. For a lung mass to cause this level of nausea and vomiting via external compression, the patient would have developed systemic symptoms. Mallory Weiss tear can explain some of our patients symptoms. She had severe nause, vomiting , retching and hematemsis. This are cardinal symptoms for this diagnosis. However, we do not have a trigger factor such as history of significant alcohol use and EGD did not show any obvious esophageal mucosal tear.
References
- Hyun JJ, Bak YT. Clinical Significance of Hiatal Hernia. Gut Liver. 5(3):267-277(2011).
- Kohn GP, Price RR, DeMeester SR, et al. Guidelines for the management of hiatal hernia. SurgEndosc.27(12):4409-4428(2013).
- Kaiser LR, Singal S. Diaphragm. In: Surgical Foundations: Essentials of Thoracic Surgery. Philadelphia: Elsevier Mosby; 294(2004).
- Miller JI Jr. Bacterial infections of the lungs and bronchial compressive disorders. In: Shields TW, LoCicero J, Reed CE, Feins RH, editors. General thoracic surgery. 7th ed.Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; (2001).
- Hill LD. Incarcerated paraesophageal hernia: a surgical emergence. Am J Surg.126(2):286-291(1973).
- Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia: long-term results with 1,030 patients. J ThoracCardiovascSurg.53(1):33-54(1967).
- Stylopoulos N, Gazelle GS, Rattner DW.Paraesophageal hernias: operation or observation?Ann Surg. 236(4):492-501(2002).
- Davis SS Jr. Current controversies in paraesophageal hernia repair. SurgClin North Am:88.(5):959-978(2008).