Immediate Effect of Neck Stabilization Exercise on Neck Repositioning Accuracy in Chronic Neck Pain Patients
- Corresponding Author:
- Ayyappan Jayavel
Assistant Professor, SRM College of Physiotherapy
SRM University, Chennai, India
Tel: 044-47432720; 044-2745-6729
E-mail: ayyappanpt@gmail.com
Abstract
Background:
Forward head posture is a musculoskeletal abnormality where the head is positioned anterior to the Line of Gravity causing neck pain, headache, temporo-mandibular disorders, myofacial pain syndrome and abnormal scapular movement.
Objectives:
To investigate the immediate effect of neck isometric exercise on neck reposition sense. Methodology: Total 19 subjects, age group 18-35 years with chronic neck pain- SRM Medical College Hospital and Research Centre, SRM University, Kattankulathur.
Intervention:
The participants were taught neck stabilization exercise. Outcome measure: Neck Reposition Sense and Numerical Pain Rating Scale.
Results and Conclusion:
In X Axis Pre Test Mean value is 8.52 and post Test Mean value is 5.66. For Y Axis Pre Test value 7.89 and Post Test value 9.78. For Numerical Pain Rating Scale Pre Test Mean value 5.84 and Post Test value is 5.15. In X Axis and in NPRS there is absolute variation and in Y Axis there is minimal change in focus is noted.
Keywords
Neck Pain, Neck stabilization exercise, Neck repositioning sense
Introduction
33% of people are reported with Neck pain every year; out of which it is estimated that 16% of the victims belong to the age group of 18 to 29 years [1]. The source of neck may be due to many varying pathologies such as whiplash, poor posture, degenerative disorders, neuropathy, tumors, surgical procedures and over working of neck muscles due to faulty postures [2-6].
Neck pain is very common in software, banking and other sedentary desk job population in recent times. This will lead to neurological deficits and sensation impairment in patients with chronic neck pain. This alters the normal and functional activities of an individual as given in recent researches.
The brain integrates information from proprioception and from the vestibular system into its overall sense of body position, movement, and acceleration. The word kinesthesia strictly means movement sense, but has been used inconsistently to refer either to proprioception alone or to the brain’s integration of proprioceptive and vestibular inputs [7-9].
Proprioception plays a major role in all the major joints with its sensory receptors and deep sensory tests. Neck extensors are the anti-gravity muscles and have the ability to maintain our head in neutral position without falling backwards. They are strained to the most in our entire life hence it is a good level to measure capacity of neck reposition [10,11].
For neck reposition sense testing, the head repositioning accuracy (HRA) test was used as it has high sensitivity score [12-15]. Pain has been reported to effect neck muscle strength, neck muscle size and thickness, range of motion, joint reposition error (JRE), and tactile acuity of cervical dermatomes [16]. Evidence suggests that the joint reposition sense is altered in neck pain patients and Reduction in maximal isometric neck strength has also been suggested, as the force production capacity is affected [17].
Hence, this study aims to identify the immediate influence of cervical stabilization exercise on joint reposition sense of the cervical kinematics in patients with chronic neck pain.
However, the efficacy of active strengthening exercises for management of chronic neck pain has been uncertain in the previous studies. In some studies, only minor or short-term improvements were induced with active exercise. In the same method this research also focuses on the immediate effect of neck reposition accuracy and improvement in their proprioception sense [18].
Methodology
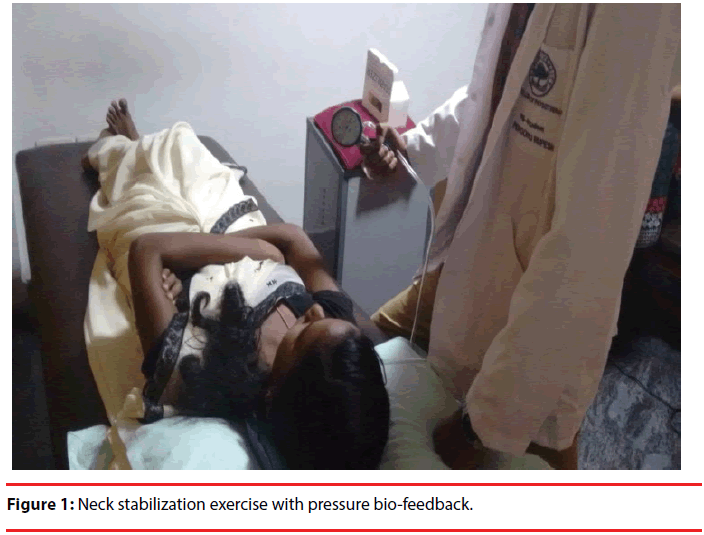
Total of 19 samples consisting of 11 males and 8 females were conveniently selected for the study. Patients with neck pain for more than 3 months, aging 18 to 35 years, with NPRS rating more than 3, were included into the study. Informed consent was taken from the patients before the trial. Patients with any neurological deficits, any recent injuries to neck and unwilling to participate were excluded from the study. Study was approved by institutional ethical committee of SRM College of Physiotherapy and was conducted in the Physiotherapy out-patient department of SRM Medical College, Hospital and Research Centre. Patients were assessed with outcome measures of pressure biofeedback, neck reposition sense and Numerical pain rating scale severity. The neck stabilization exercise protocol [19] was followed with rest intervals and the post-test values of the same were noted.
The patients were instructed to stand with their feet at shoulder width distance, and sit upright on the chair without leaning over, wearing a helmet fitted with laser probe and asked to focus a particular point on a 2×2 feet printed graph sheet, placed at a distance of 2 meters. The focus point was noted as X and Y. Then instructions to flex the neck at an angle of 30 degrees, holding the pose for 3 seconds and aim to focus on to the same point (X1, Y1) were given, while the therapists marked the points. Then patients positioned in supine lying were taught neck stabilization exercises with 15 seconds holding time and 10 repetitions per set, for a total of 3 sets.
Between each repetition the subject took 10 seconds break and between each set the subject took 1 minute break. The patients were asked to tuck their chin and press the stabilizer placed behind the neck, so that the pressure could be kept at 30 mm Hg [20]. The Chattanooga pressure biofeedback apparatus was used for the visual feedback to the patient and maintained at the pressure of 30 mm Hg. Finally for the post test readings, the patients were instructed to repeat the pre-test procedure and the therapists marked the points, of which the differences of X, X1 and Y, Y1 values were recorded from the graph.
Results
For X axis, there is Statistical significance difference at 95% Confidence Interval (P=0.000, t=10.03,) with Pre Test Mean value is 8.52 and post Test Mean value is 5.66 (Table 1). For Y axis there is Statistical significance difference at 95% Confidence Interval (P=.000, t=-4.86) with Pre Test value 7.89 and Post Test value 9.78. For Numerical Pain Rating Scale there is Statistical significance difference at 95% Confidence Interval (P=.003, t=3.36) with Pre Test Mean value 5.84 and Post Test value is 5.153 (Table 2).
| Mean | Standard Deviation | t Test | P Value | ||
|---|---|---|---|---|---|
| X Axis | Pre Test | 8.52 | 1.57 | 10.03 | 0.000* |
| Post Test | 5.66 | 1.73 | |||
| Y Axis | Pre Test | 7.89 | 3.68 | -4.86 | 0.000* |
| Post Test | 9.78 | 3.67 | |||
*There is Statistical significance difference in X Axis and Y Axis at 95% Confidence Interval [P < 0.05]’
Table 1: Difference of Pre Test and Post Test Mean values of X and Y Axes.
| NPRS | Mean | Standard Deviation | t Test | P Value |
|---|---|---|---|---|
| Pre Test | 5.84 | 0.89 | 3.36 | 0.003* |
| Post Test | 5.15 | 1.25 |
*There is Statistical significance difference in NPRS at 95% Confidence Interval [P < 0.05].
Table 2: Difference of Pre Test and Post Test Mean values of NPRS.
Discussion
As the neck provides connectivity between head and body and it has both stability as well as mobility functions, any habitual bad posture and repetitive strain will result in minute injuries gradually leading to neck pain [21]. Chronic neck pain patients frequently face formation of straightened neck of backward flexion due to the structural deformation of cervical vertebra which may result in neck pain [21].
Taimela reported that the head repositioning accuracy of chronic neck pain patients was lower than that of normal person [22].
Sensation and neck position sense are two of the most important functions of the neck. As the body’s center for controlling balance is located within the inner ear, neck position sense is vital in the control and maintenance of balance [23]. Increased understanding of the effect neck pain has on neck position sense has led to a recent increase in the study of vestibular rehabilitation as a treatment of neck pain. This suggests that neck pain sufferers may benefit from training exercises designed to improve neck position sense [24-26]. The Joint Reposition Error test offers an inexpensive and quick method of clinically measuring neck position sense [27].
Revel et al. in the initial study examining JRE reported little difference was found between the pain and no pain groups with horizontal movements with a reported error of 3.37º ± 0.73º in the pain group. Since the work by Revel [27], several studies have been performed to establish normative values for JRE on each of the three cardinal planes both in healthy controls and in patients suffering from neck pain [27]. In this study, though, it was found that there was significant difference in sagittal plane (p=0.00) and highly significant difference in the coronal plane (p= 0.000) between the two cardinal planes considered (Figure 1).
The analyzed results are based on the neck reposition accuracy and in two of the readings (X Axis and Y Axis) coronal plane and in sagittal plane respectively, the relation with is nearly matching in X Axis and in Y Axis there is increase in height of accuracy than previous point. There is no notable change in the Numerical Pain Rating Scale severity. Teng examined the effects of age on cervical JRE. They reported that there was a significant difference in JRE in middle aged adults when compared to young adults regardless of neck pain [28]. Therefore, we attempted to investigate the immediate effect of neck stabilization exercise and the variances in reposition error due to pain level in adults suffering neck pain (Figure 2).
Jung confirmed that the sense of joint position, when bending and extending the neck at a sitting posture had significantly less deviation in the upright posture than the bending posture [29]. Though the present study was aimed at promoting the proprioception by recovering the normal posture of neck joint through the cervical stabilization exercise, it could not identify the change in promotion due to the too short term of exercise. Jull [25], examined the effect of proprioception training in patients with chronic neck pain, reported significant decreases in JRE, perceived neck pain and perceived disability in both groups. Due to the lack of availability of research in this area further investigation is needed to determine the effectiveness of neck position sense and tactile acuity training programs in the treatment of chronic neck pain [25].
Conventional physical therapy programs use a combination of strength training and range of motion exercises to treat patients with neck pain have shown that strength training along with stretching has decreased pain in chronic neck pain sufferers. However, the effect of proprioception training is less understood [30-36]. Using this information, this study focused on an exercise for catering to proprioception other than the usual exercises for improving the neck range of motion and strength, for the overall neck function. This was obtained to counteract the negative effects of pain on joint reposition sense and tactile acuity. Thus, exercises involving neck position sense should be incorporated as part of treatment procedures when treating patients suffering from chronic neck pain is recommended [37].
Limitations of this study include less sample size, short study duration and lack of neck exercise protocol followed as stabilization exercise was only focused. From this study, further investigations on large population, longer duration, additional neck strengthening, effect on scapular position, randomized sampling technique, over-head sport athletes, occupations involving more overhead activities are recommended.
Conclusion
In this study, it was found out that cervical stabilization exercises helped reduce the problem related to head repositioning accuracy, with identified statistical significance. Thus, exercises involving neck position sense should be incorporated as part of treatment procedures when treating patients suffering from chronic neck pain is recommended.
Acknowledgement
I would like to extend my deep sense of gratitude towards SRM Management, SRM College of Physiotherapy and patients, for their support throughout my study duration.
References
- Croft PR, Lewis M, Papageorgiou AC,et al.Risk factors for neck pain: A longitudinal study in the general population. Pain 93(3), 317-325 (2001).
- Sjölander P, Michaelson P, Jaric S, et al.Sensorimotor disturbances in chronic neck pain–range of motion, peak velocity, smoothness of movement, and repositioning acuity.Man. Ther13(2), 122-131.
- Yoo WG, An DH. The relationship between the active cervical range of motion and changes in head and neck posture after continuous VDT work. Ind. Health47(2), 183-188 (2009).
- Baron R. Peripheral neuropathic pain: From mechanisms to symptoms. Clin. J. Pain16(2), S12-S20.
- Krnam P, Suresh A, Trivedi N, et al.Persistent pain as a prognostic factor of residual/recurrent tumor in head and neck cancer. Oral.Oncol47:S142-S142(2011).
- Takeuchi K,Yokoyama T, OnoA, et al.Limitation of activities of daily living accompanying reduced neck mobility after laminoplasty preserving or reattaching the semispinaliscervicis into axis. Eur. Spine. J17(3), 415-420.
- Proske U, Gandevia SC.The kinaesthetic senses.J. Physiol587 (17), 4139-4146.
- WinterJA, TJ Allen, U Proske.Muscle spindle signals combine with the senses of effort to indicate limb position. The journal of physiology 568(pt 3), 1035-1046.
- Collins DF, Refshauge KM, Todd G, et al.Cutaneous receptors contribute to kinesthesia at the index finger, elbow and knee. J.Neurophysiol94 (3), 1699-1706.
- Lee HS, Chung HK, ParkSW. Correlation between trunk posture and neck reposition sense among subjects with forward head neck postures. BioMed. Res. IntArticle ID 689610, 6 (2015).
- Barton PM, Hayes KC. Neck flexor muscle strength, efficiency, and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch. Phys. Med. Rehabil77(7), 680-687 (1996).
- CagnieB, Cools A, De Loose V. Differences in isometric neck muscle strength between healthy controls and women with chronic neck pain: The use of a reliable measurement. Arch. Phys. Med. Rehabil88(11), 1441-1445 (2007).
- Rezasoltani A, Ahmadipoor A, Khademi-Kalantari K, et al.The sign of unilateral neck semispinaliscapitis muscle atrophy in patients with chronic non-specific neck pain. J. Back.Musculoskelet.Rehabil25(1), 67-72 (2012).
- McPartland JM, Brodeur RR, Hallgren RC. Chronic neck pain, standing balance, and suboccipital muscle–A pilot study. J. Manipulative. Physiol. Ther20(1),24-29 (1997).
- Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine (Phila Pa 1976) 29(1), 33-40 (2004).
- Highland TR, Dreisinger TE, Vie LL, et al.Changes in isometric strength and range of motion of the isolated cervical spine after eight week of clinical rehabilitation. Spine (Phila Pa 1976)17: 77-82 (1992).
- Kang KW, KangDW, Kwon GE. The impact of head repositioning accuracy and proprioception on cervical stabilization exercise in healthy adults.Phys.Ther.Rehabil.Sci4 (1), 49-54 (2015).
- Kisner C, Colby LA. Therapeutic exercise: foundations and techniques. (4th edn) Philadelphia: FA Davis (1985).
- Boyd-Clark LC, Briggs CA, Galea MP. Muscle spindle distribution, morphology, and density in longuscolli and multifidus muscles of the cervical spine. Spine (Phila Pa 1976)27, 694-701 (2002).
- Taimela S, Takala EP, Asklöf T, et al.Active treatment of chronic neck pain: a prospective randomized intervention. Spine (Phila Pa 1976)25(8), 1021-1027 (2000).
- Armstrong B, McNair P, Taylor D. Head and neck position sense. Sports. Med38(2), 101-117 (2008).
- Hansson EE, Persson L, Malmstrom EM. Influence of vestibular rehabilitation on neck pain and cervical range of motion among patients with whiplash-associated disorder: A randomized controlled trial. J. Rehabil. Med 45(9), 906-910 (2013).
- Jull G, Falla D, Treleaven J, Hodges P, et al.Retraining cervical joint position sense: The effect of two exercise regimes. J.Orthop. Res25(3), 404-412(2007).
- Revel M, Minguet M, Gergoy P, et al.Changes in cervicocephalickinesthesia after a proprioceptive rehabilitation program in patients with neck pain–A randomized controlled study. Arch. Phys. Med. Rehabil75(8), 895-899 (1994).
- Revel M, Andredeshays C, Minguet M. Cervicocephalickinestheticsensability in patients with cervical pain. Arch. Phys. Med. Rehabil72(5), 288-291 (1991).
- Teng CC, Chai H, Lai DM, et al.Cervicocephalickinesthetic sensibility in young and middle-aged adults with or without a history of mild neck pain. Man.Ther 12(1), 22-28 (2007).
- Jung JM, Gu JS, Shin WS. The effect of different sitting postures on range of motion, strength and proprioceptive sense of neck. J. Korea.Acad-Ind. Coop13:2212-2218 (2012).
- Highland TR, Dreisinger TE, Vie LL, et al.Changes in isometric strength and range of motion of the isolated cervical-spine after 8 weeks of clinical rehabilitation. Spine (Phila Pa 1976)17(6), S77-S82 (1982).
- Hakkinen A, Salo P, Tarvainen U, et al.Effect of manual therapy and stretching on neck muscle strength and mobility in chronic neck pain. J.Rehabil. Med39(7), 575-579 (2007).
- Ylinen JJ, Takala EP, Nykanen MJ, et al.Effects of twelve-month strength training subsequent to twelve-month stretching exercise in treatment of chronic neck pain. J. Strength. Cond. Res20(2), 304-308.
- Salo P, Ylinen J, Kautiainen H, et al. Neck muscle strength and mobility of the cervical spine as predictors of neck pain: A prospective 6-year study. Spine (Phila Pa 1976)37(12), 1036-1040.
- Ylinen J, Kautiainen H, Wiren K, et al.Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross-over trial. J.Rehabil. Med39(2), 126-132.
- Bunketorp L, Lindh M, Carlsson J, et al.The effectiveness of a supervised physical training model tailored to the individual needs of patients with whiplashassociated disorders–A randomized controlled trial. Clin. Reh20(3), 201-217.
- Miller J, Gross A, D'Sylva J, et al. Manual therapy and exercise for neck pain: A systematic review. Man.Ther15(4), 334-354.
- Kristjansson E, Dall'Alba P, Jull G. A study of five cervicopephalic relocation tests in three different subject groups.Clin.Rehabil17(7), 768-774.
- Mosby's Medical, Nursing & Allied Health Dictionary, 4th (edn), Mosby-Year Book p. 1285
- Tamura Y, Hoshiyama M, Inui K.Central mechanisms for two-point discrimination in humans. Neurosci. Lett342(3), 187-190 (2003).